Wednesday Slide Conference, Conference 4, Case 1
Signalment:
4.5 month old, 27 kg neutered male pig (Sus scrofa domesticus).
History:
This pig arrived from a facility that had an outbreak of Staphylococcus hyicus, with several animals arriving with small lesions on the pinna, or developing lesions after arrival. Lesions progressed the longer the animals were housed in our facility.
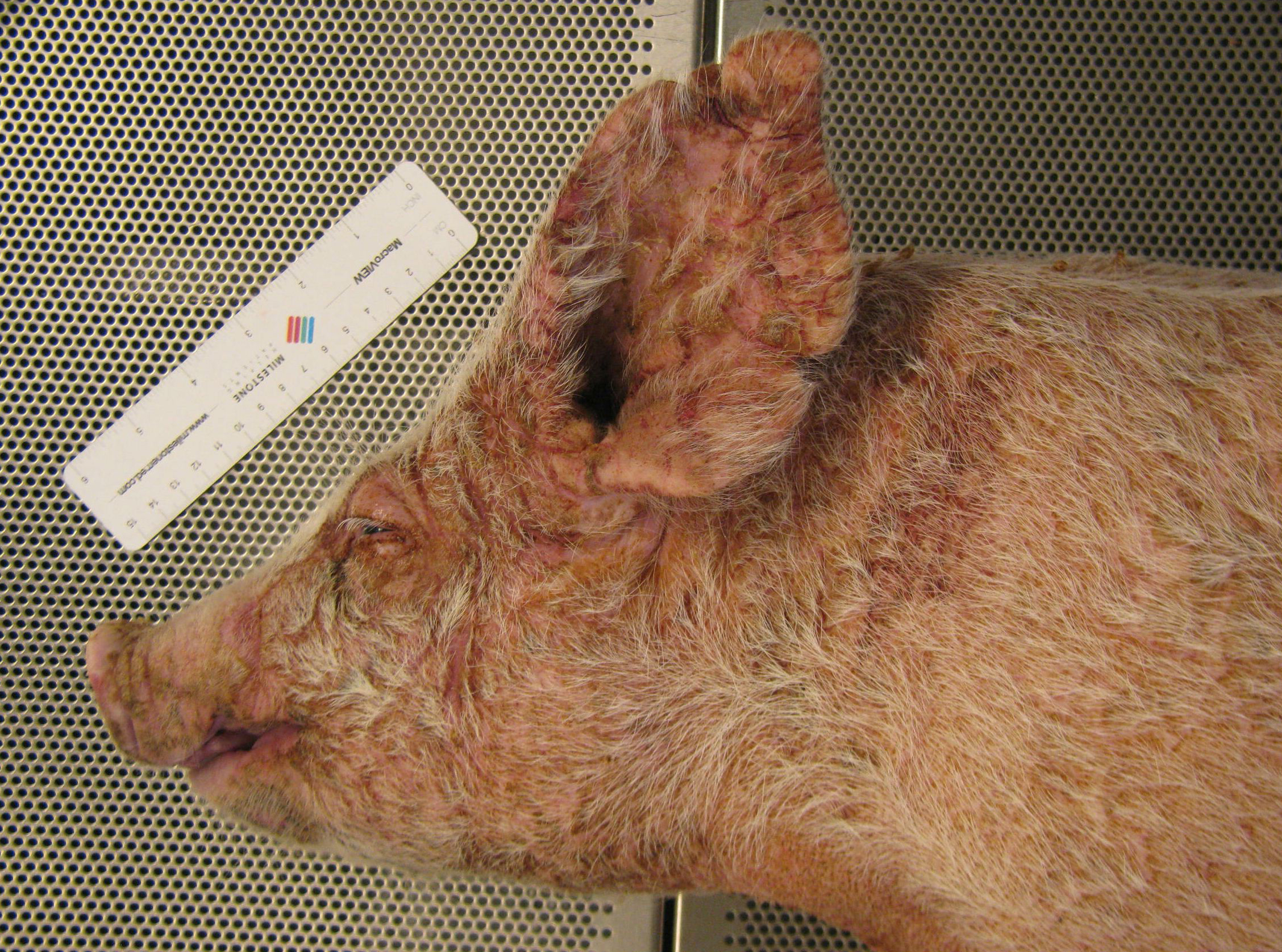
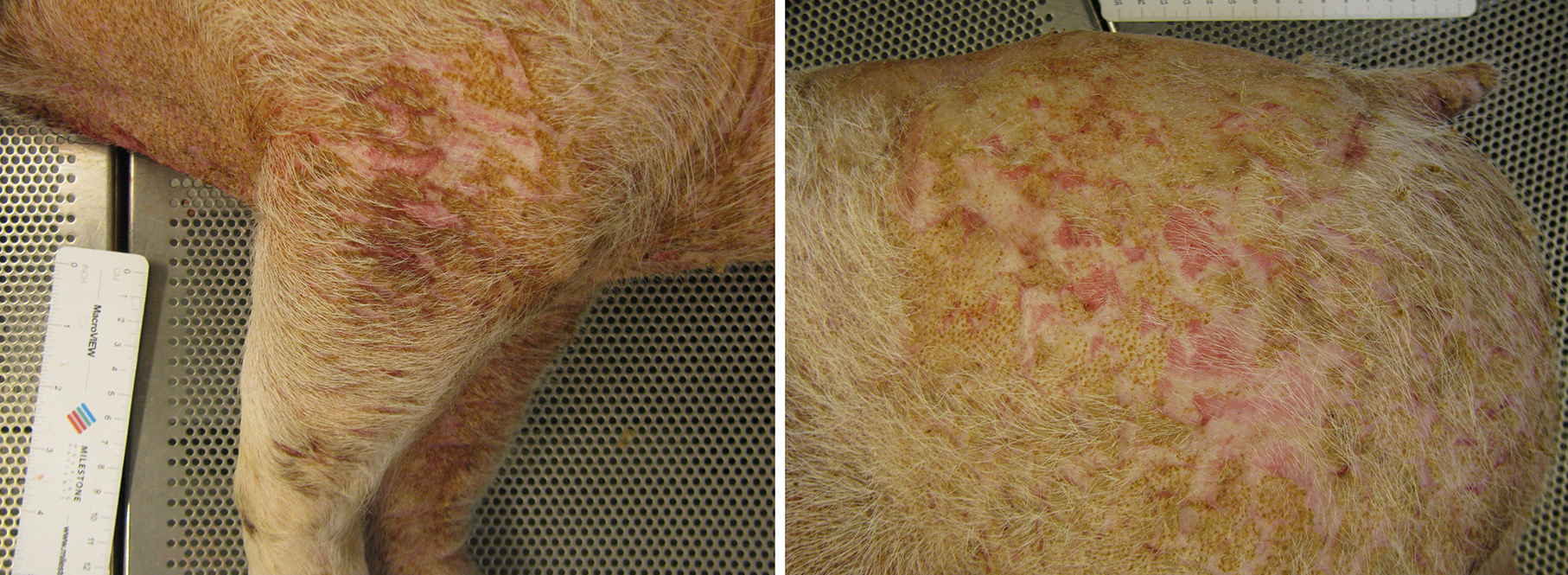
Gross Pathology:
There is multifocal, regionally extensive erosion, erythema, and crusting affecting the head, pinna, the lateral left leg, and the lateral rump. There is moderate exudation and hypotrichosis in affected areas, with mild lichenification and fissures in the most severely affected regions.
Laboratory Results:
Gram stains show numerous colonies of gram positive cocci and gram negative bacilli within crusts, and extending into follicles.
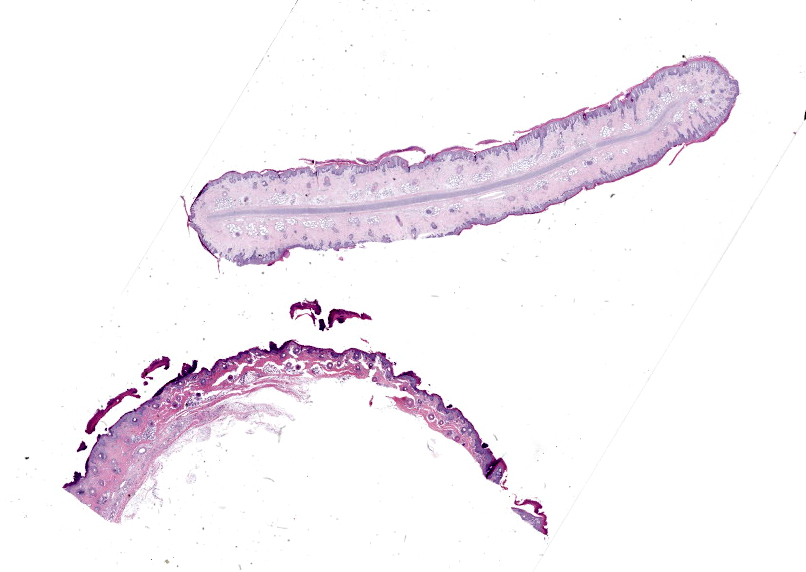
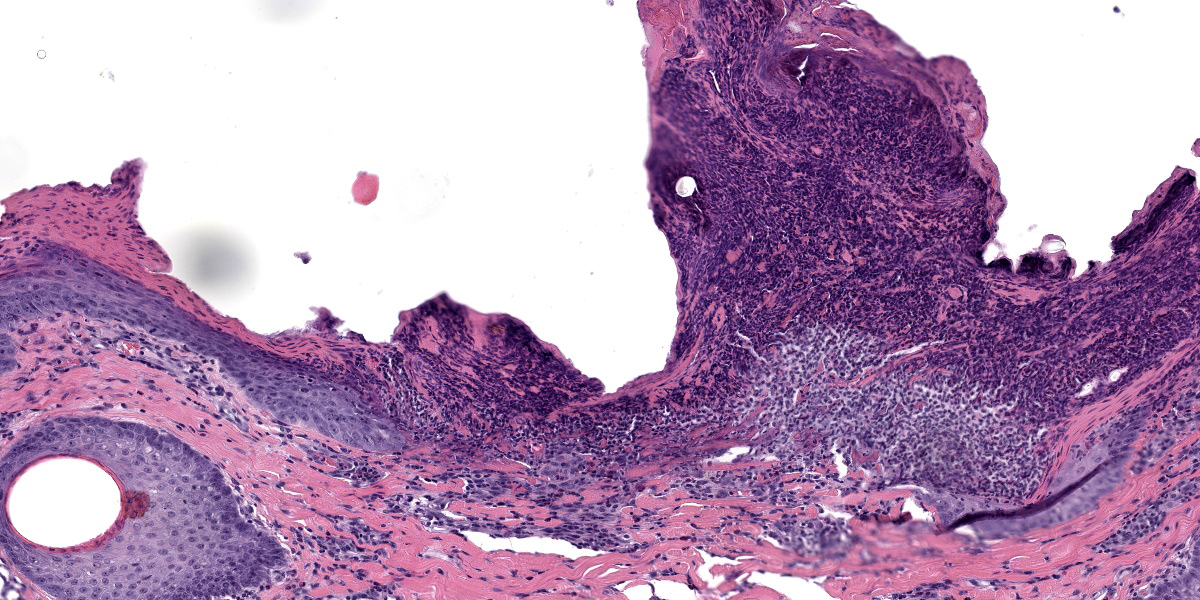
Microscopic Description:
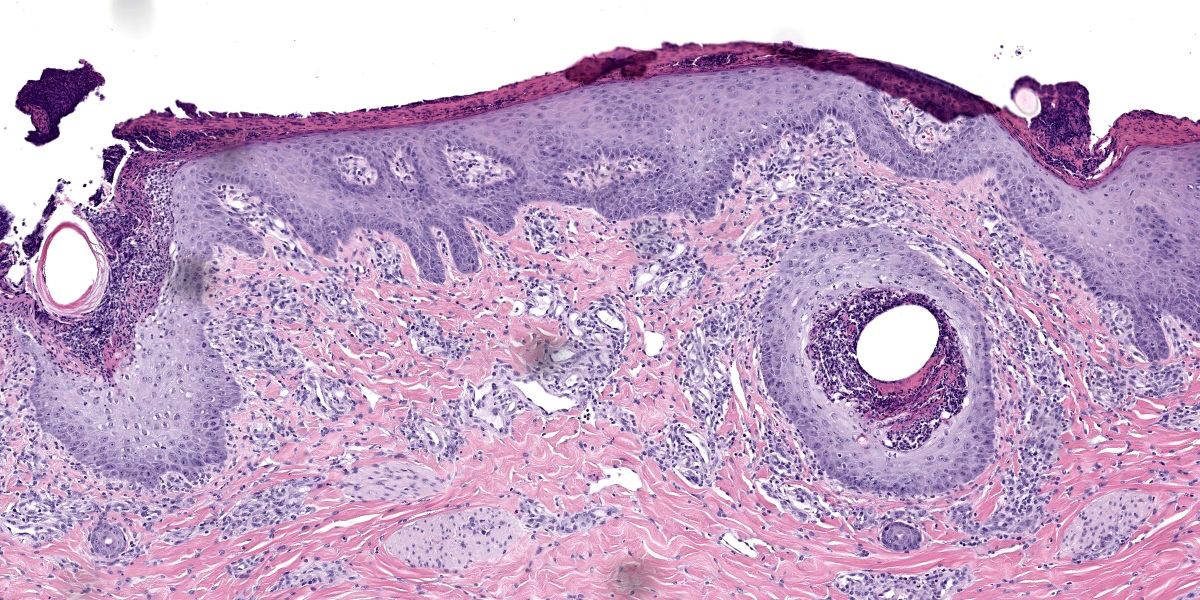
Haired skin, pinna and unspecified site: Affecting approximately 90% of the section, there is marked parakeratotic hyperkeratosis, with multifocal intracorneal pustules composed of necrotic cellular debris, necrotic neutrophils, and often individual to colonies of 1 um diameter basophilic cocci. There is multifocal elevation of the necrotic debris, forming a serocellular crust. There is multifocal ulceration, with necrosis of both the epidermis and subjacent dermis. Within the hyperplastic stratum corneum are also multifocal lakes of serum, transmigrating neutrophils, and degenerating and necrotic keratinocytes. Subjacent to the stratum corneum, there is marked acanthosis, with prominent intercellular and intracellular edema, and deep anastomosing rete ridges extending to the mid dermis. Follicles are multifocally dilated with luminal neutrophilic debris admixed with cocci adherent to the inner follicular epithelium. Within the dermis, there are perivascular to superficial histiocytic and eosinophilic infiltrates, fewer lymphocytes and plasma cells, and mildly increased white space between bundles of collagen (edema). Multifocal lymphatics are ectatic, and apocrine glands are ectatic with attenuated epithelium.
Brown and Brenn stain: There are individual and colonies of gram positive cocci within the serocellular crusts, stratum corneum, and adherent to luminal follicular epithelium. There are also gram negative bacilli admixed with gram positive cocci.
Contributor’s Morphologic Diagnosis:
- Haired skin, multiple locations including ear: Epidermitis, exudative and proliferative, diffuse, severe, with intracorneal pustules, rare ulceration, mild chronic active superficial dermatitis, and intracorneal cocci, breed not specified, swine.
- (Not submitted) Lymph nodes, multiple: No significant findings.
Contributor’s Comment:
Exudative epidermitis, or “greasy-pig disease”, primarily affects 5-35 day old piglets and is caused by Staphylococcus hyicus. The condition is also known as impetigo contagiosa suis, and seborrhea oleosa, and is occasionally caused by Staphylococcus chromogenes or Staphylococcus sciuri.6 While this disease can have high morbidity and variable mortality, this is considered an important disease due to economic loss.6 The bacterium is considered a commensal organism that survives on the skin and within hair follicles, most often not causing disease. However, with compromise to immune function from environmental stressors like overcrowding, transport, poor husbandry, an individual animal’s susceptibility to this disease may increase.8 If not strictly required, it is currently thought that damage to the epidermis from fighting, abrasions from housing, ectoparasitism, or concurrent vesicular disease allows entry of S. hyicus for colonization.2
The disease is classically categorized into three different presentations. In the acute form, lesions around the eyes, snout, chin, and ears appear rapidly, then spread to the medial aspect of the legs, thorax, abdomen, and coronets. As the stratum corneum of affected regions peels away, moist underlying epidermis and dermis are replaced by greasy, dark brown exudate. In the subacute form, the progression of disease is slower, resulting in thick, wrinkled skin that eventually shows a generalized furrowed appearance. The chronic form affects older piglets, with milder disease, usually erythema and waxy brown crusts confined to the head and ears. Older piglets often survive the disease but may have stunted growth.6
The most important virulence factors identified to date include a number of exfoliative toxins, ExhA, ExhB, ExhC, ExhD, SHETA, and SHETB. The Exh family toxins digest desmoglein-1 in the epidermis, affecting the effectiveness of desmosomes.6 There are also a number of fibronectin-binding proteins on the surface of the bacteria that allow for adhesion to fibronectin in collagen, fibrin, and heparan sulfate proteoglycans found in the skin. Once the bacteria are established in the dermis, the infection often spreads to hair follicles, causing suppurative dermatitis with sebaceous gland hyperplasia and increased secretion (i.e. the “greasy” aspect of the disease).7
Lesions usually progress to exudative dermatitis starting in the groin, axillae, caudal auricular, and traumatized areas. Haired areas are more often affected, but lesions may also arise on the tongue and oral mucosa.2 While not specific for the disease, a number of histologic features would support the diagnosis, such as subcorneal vesicular to pustular dermatitis, purulent luminal folliculitis, variable acanthosis with elongated rete ridges, intracellular edema of the stratum spinosum, and orthokeratotic and parakeratotic crusts with lakes of serum, accumulations of neutrophils, debris, and colonies of gram-positive cocci.6
The virulence and antibiotic resistance of S. hyicus continues to change as a function of its environment. A comparison of isolates from Brazilian swine herds in the 1980’s and 2012 highlights significant shifts of ExhA and ExhB expression, as well as different antibiotic resistance profiles.7 As antimicrobial peptides are investigated to combat increasing antibiotic resistance to macrolides, B-lactams, tetracycline, sulfonamides, and streptomycin, some compounds such as lactoferricin (Lfcin) have recently shown effectiveness in treating S. hyicus in a mouse model. Lfcin disrupts the bacterial cell wall and was effective in reducing both the bacterial load and levels of pro-inflammatory cytokines TNF-a, IL-6, and IL-1B.4 Other biologics with efficacy have been recently investigated as well, such as the insect defensin DLP4 from Hermetia illucens (black soldier fly),5 fungal defensin NZL from Pseudoplectania nigrella,3 and Siphoviridae-like bacteriophages.9
Contributing Institution:
Walter Reed Army Institute of Research
Department of Pathology
https://www.wrair.army.mil/
JPC Diagnosis:
Haired skin: Epidermitis and folliculitis, suppurative, subacute, diffuse, severe, with multifocal ulceration, pustules, and intracorneal cocci.
JPC Comment:
The moderator for this week’s conference was Major Kelsey Fiddes who serves as the Chief of Resident Training at the JPC. Each year, conference 4 is the annual rite of passage for our new first-year residents, presenting their first WSC case. This first case is a classic entity that we have covered in WSC before (Case 1, Conference 9, 2008-2009 and Case 3, Conference 8, 2009-2010) and the supplied section supplied is diagnostically rewarding.
As the contributor notes, the sebaceous gland hyperplasia elicited by S. hyicus may be the most visually obvious clue of this disease grossly, but there are several histologic features that should not be overlooked (Figures 1-4 and 1-5). In particular, the changes within the follicular infundibulum spanning the lumen and wall led us to include folliculitis with our morphologic diagnosis. In addition, the morphologic diagnosis focuses on epidermal changes, as the underlying dermis lacks significant changes. Gram stains (not particularly necessary in this case) highlight cocci within the serocellular crusts, stratum corneum, and adherent to luminal follicular epithelium similar to what the contributor reports.
As the contributor summarizes, the exfoliative toxins of S. hyicus play an important role in the pathogenesis of this disease. Other staphylococci such as S. aureus also produce serine protease exfoliative toxins;1 these have been associated with human cases of bullous impetigo and staphylococcal “scalded skin syndrome”6 which bear some similarity to exudative epidermitis of pigs. Microscopic lesions may be seen in other tissues due to exfoliative toxins. Renal lesions, including degeneration and/or exfoliation of the tubular epithelium, are a common sequela and do not require concurrent bacteremia. In cases of bacteremia, purulent pyelonephritis is a common finding6 though it should be distinguished from other potential causes (e.g. Actinobacillus) that have a different pathogenesis.
References:
- Bukowski M, Wladyka B, Dubin G. Exfoliative Toxins of Staphylococcus aureus. Toxins. 2010; 2(5):1148-1165.
- Helke KL, Ezell PC, Duran-Struuck R, Swindle MM. Biology and Diseases of Swine. In: Fox JG, et al. eds. Laboratory Animal Medicine. 3rd ed. San Diego, CA: Elsevier. 2015:742-743.
- Lui H, Yang N, Teng D, et al. Design and pharmacodynamics of recombinant fungus defensin NZL with improved activity against Staphylococcus hyicus in vitro and in vivo. Int. J. Mol. Sci. 2021; 22:5435.
- Liu H, Yang N, Teng D, et al. Fatty acid modified-antimicrobial peptide analogues with potent antimicrobial activity and topical therapeutic efficacy against Staphylococcus hyicus. Applied Microbiology and Biotechnology. 2021; 105: 5845–5859.
- Ma X, Yang N, Mao R, et al. The pharmacodynamics study of insect defensin DLP4 against toxigenic Staphylococcus hyicus ACCC 61734 in vitro and vivo. Front Cell Infect Microbiol. 2021; 11:638598.
- Mauldin EA, Peters-Kennedy J. Integumentary System. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals, Vol 3. 6th ed. Philadelphia, PA: Saunders Elsevier; 2016:630-632.
- Moreno AM, Moreno LZ, Poor AP, et al. Antimicrobial resistance profile of Staphylococcus hyicus strains isolated from Brazilian swine herds. Antibiotics. 2022; 11(2):205.
- Stanton JB, Zachary JF. Mechanisms of Microbial Infections. In: McGavin MD, Zachary JF, eds. Pathologic Basis of Veterinary Disease. 6th ed. St. Louis, MO: Elsevier; 2017:235.
- Tetens J, Sprotte S, Thimm G, et al. First molecular characterization of Siphoviridae-like bacteriophages infecting Staphylococcus hyicus in a case of exudative epidermitis. Front. Microbiol. 2021; 12:653501.