Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2017-2018
Conference 1
August 23rd, 2017
CASE IV: UMC171 (JPC 4099789).
Signalment: Sixteen-year-old, neutered male, Domestic shorthair cat (Felis catus).
History: The cat had an enlarged thyroid discovered during dental prophylaxis 1.5 years before death. At this time there was a grade I murmur auscultated over the left heart. Anti-thyroid medication was started but was discontinued due to miscommunication with the owner about the need for life-long therapy. Four months before euthanasia the cat was noted to be losing weight and was presented again. It was treated for hyperthyroidism and hypertension. Three weeks before euthanasia, the cat became depressed and painful over several days and was brought to an emergency service. He was found to have hyphema in both eyes, with elevated intraocular pressure in the left eye. BUN was also increased. After several days of trying unsuccessful medical therapy and pain relief, the cat was euthanized. The cardiac murmur had become grade IV of VI at three days before euthanasia.
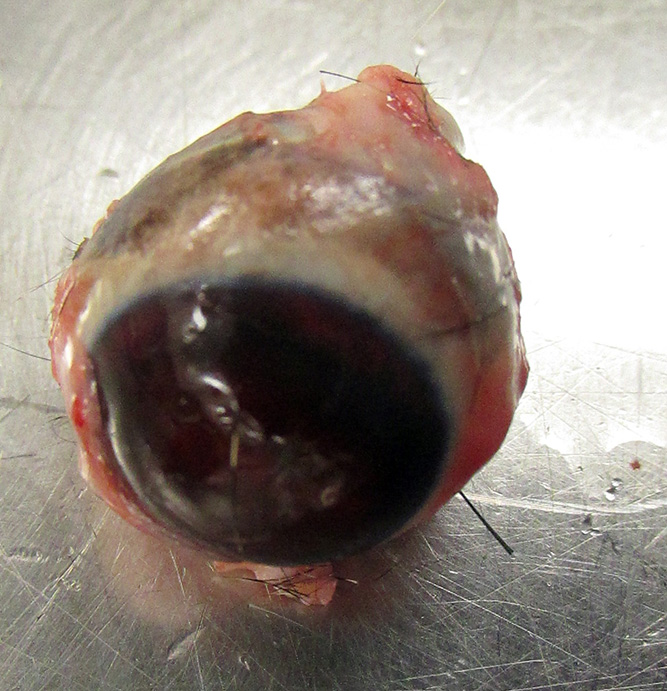
Gross Pathology: An aged, neutered male, silver tabby and white, short-haired feline is necropsied. The animal has body weight 4.6 kg, with adequate fat stores and minimal autolysis. The left eye is filled with blood, and the cornea bulges forward. An ulcer covers the central cornea. Blood leaks into the fixative when the eye is immersed in formalin after removal. The left thyroid is dark brown in color and enlarged, with a length of 1.5 cm. The right thyroid is reduced in size, nodular, and atrophic. The parathyroid glands are prominent. The kidneys are pale tan in color with a slight indentation of the anterior pole of the left kidney. They are firm in texture and the cortex has a somewhat granular character, with reduced cortical width. The combined kidneys weigh 33.5 grams, 0.72% body weight (normal 1.1%).The heart, especially the left ventricle, is severely enlarged. The total heart weight is 25.2 grams, 0.54% body weight. The right ventricular free wall weighs 3.0 grams (11.0% total heart weight) and the left ventricle weight 16.0 grams (63% heart weight, .35% body weight). The left to right ventricular weight ratio is 5.33, increased). The right ventricular wall measures 2 mm in width and the left 11 mm (ratio 5.5, increased).
Gross Morphologic Diagnosis: None provided.
Laboratory results:
|
Weeks pre-euthanasia |
BUN |
Creat |
Na |
Cl |
K |
T4 |
BP |
IOC |
|
Reference Range |
17-35 mg/dL |
0.5-2.2 mg/dL |
149-159 mEq/L |
114-122 mEq/L |
3-4.7 mEq/L |
0.8-4.0 ug/L |
120 mm HG systolic |
19.7± 5.6 mmHg |
|
1 year |
40 |
2.6 |
153 |
116 |
2.8 |
- |
186 |
- |
|
16 weeks |
46 |
1.8 |
146 |
111 |
03.2 |
7.4 |
- |
- |
|
3 weeks |
43 |
2.3 |
152 |
118 |
2.9 |
4.7 |
250 |
40 OD |
|
2 weeks |
35 |
2.3 |
154 |
3.5 |
119 |
- |
148 |
- |
|
3 days |
96 |
5.1 |
149 |
108 |
3 |
3.9 |
150 |
- |
|
1 day |
65 |
2.9 |
162 |
122 |
2.8 |
- |
168 |
- |
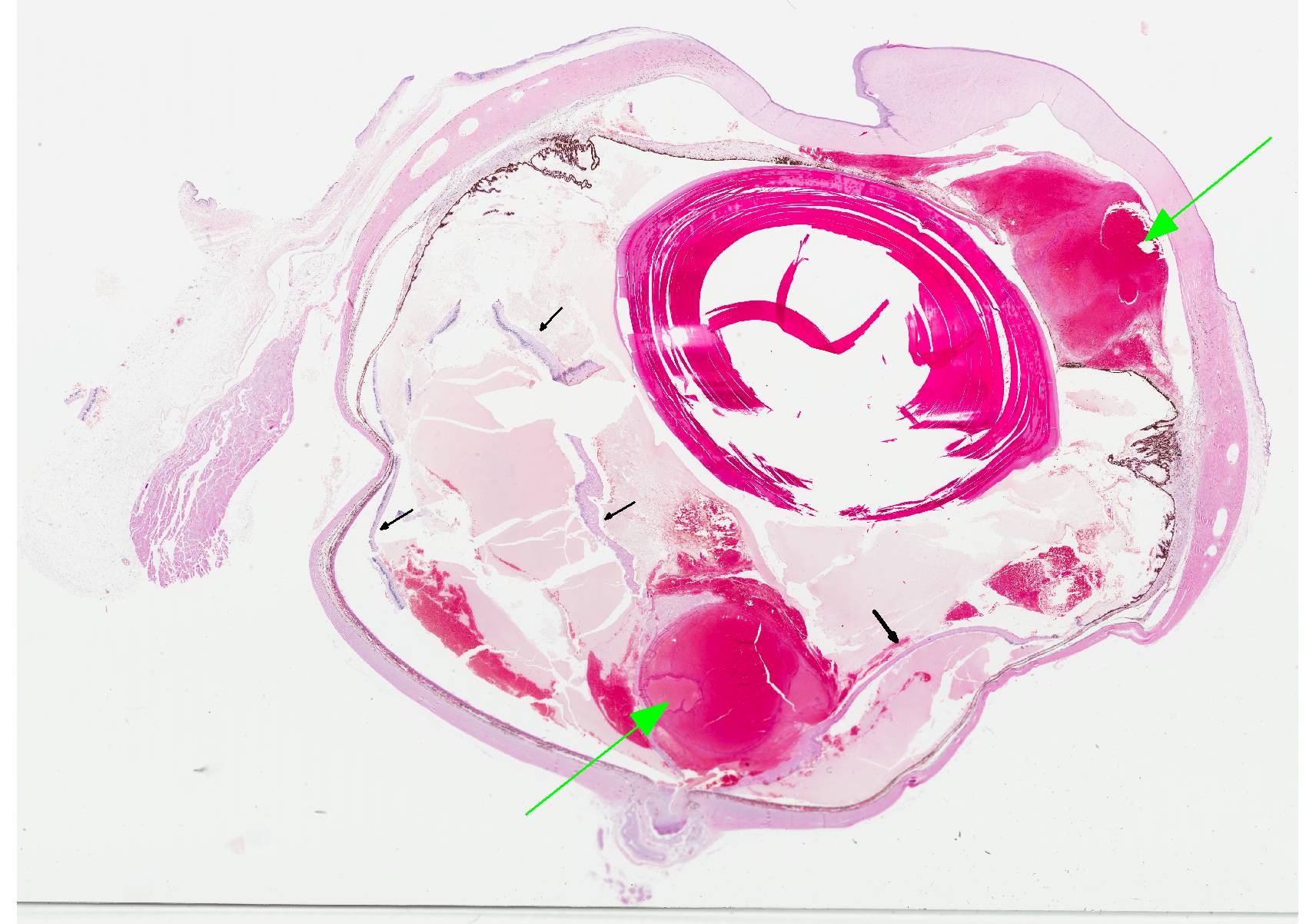
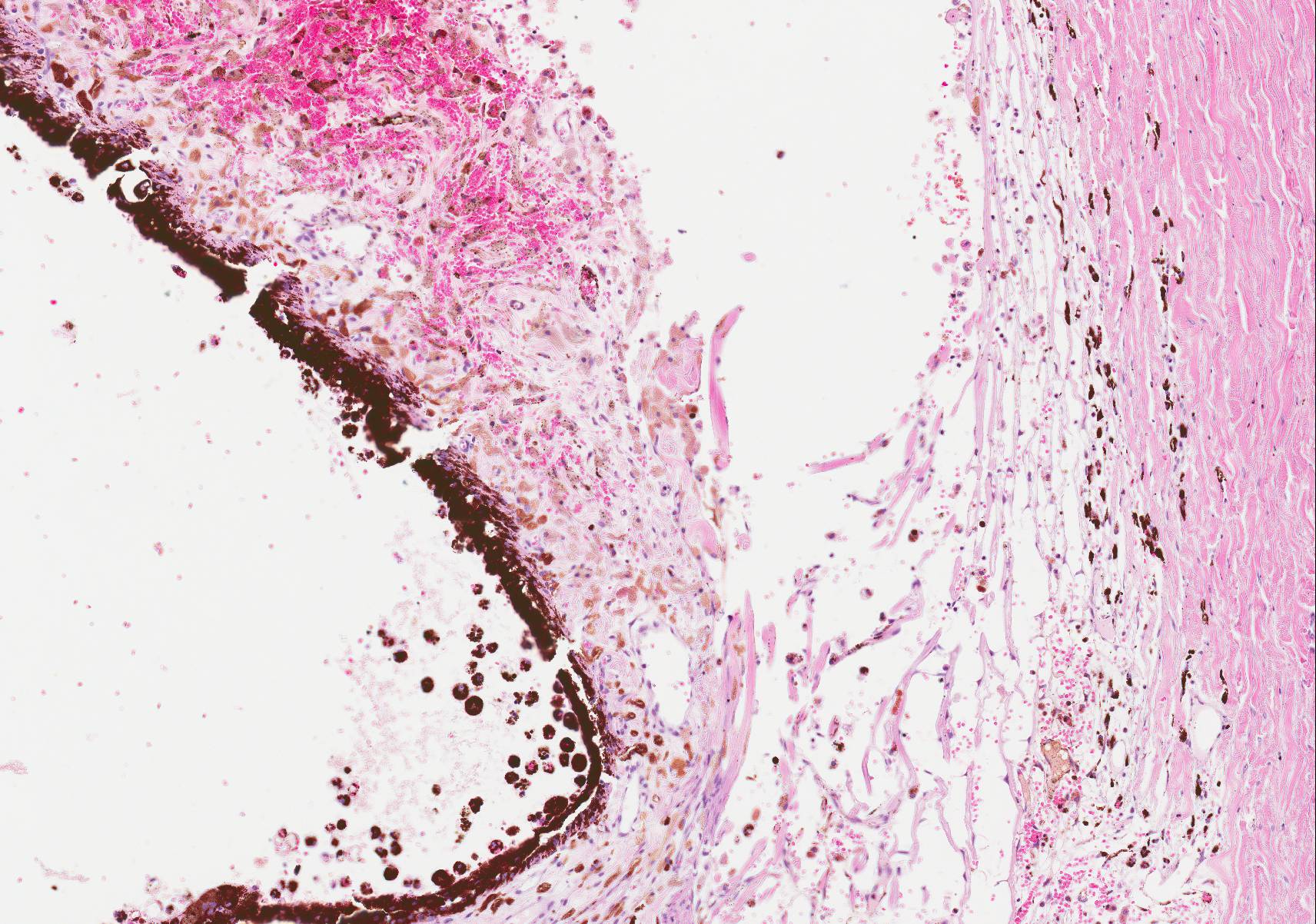
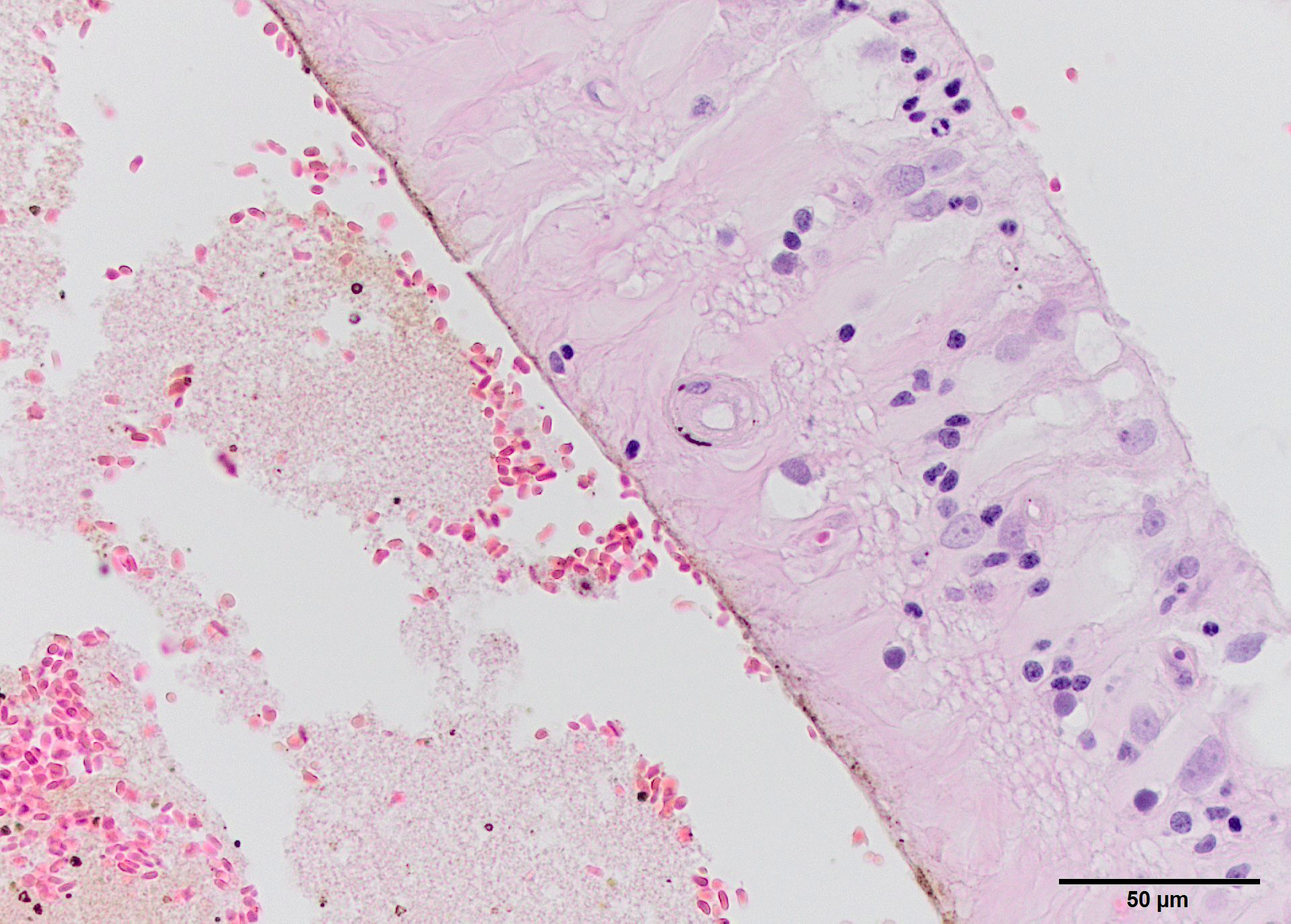
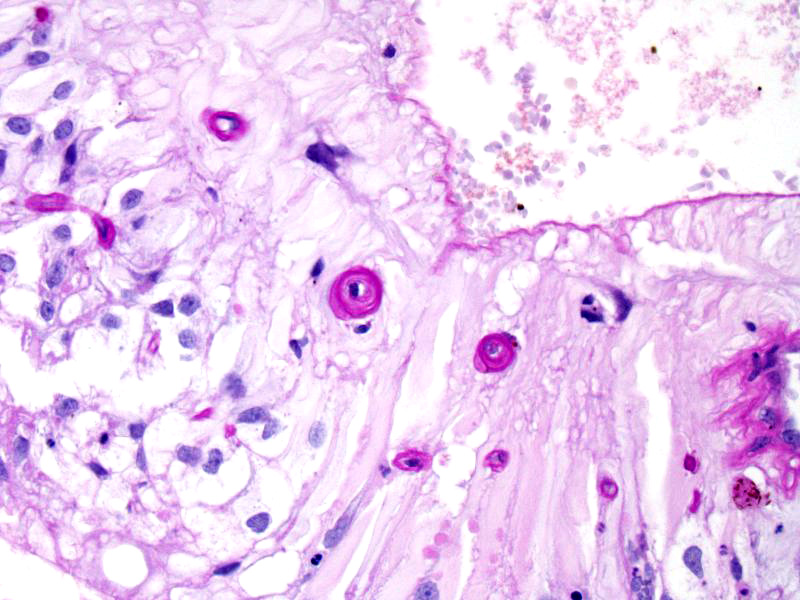
Microscopic Description: The anterior portion of the eye is filled with hemorrhage, including the angle, with extensive hemosiderosis at the root of the iris and in the meshwork. Additional hemorrhage mixes with the vitreous in parts of the posterior chamber and lies on both sides of a detached retina. The RPE is universally hypertrophic. The detached retina is severely atrophic, with reduction and mixing of the granular layers and with loss of the ganglion cells, particularly at the periphery. Scattered hemosiderophages are also present in the retina and small arterioles are thickened. Adjacent optic nerve contains few axons (not present in all slides). Thick, hyalinized arterioles occur in the choroid and retina. PAS staining highlights increased eosinophilic material in the media of small muscular vessels. A segment of corneal erosion is attended by stromal disarray, melanosis and vascularization, with mild superficial inflammation. A narrow fibrovascular membrane extends along the anterior face of the iris.
Contributors Morphologic Diagnoses: Hyphema with glaucoma, retinal detachment, retinal atrophy and corneal erosion with keratitis
Arteriolar degeneration (arteriolosclerosis), eye
Other pertinent final diagnoses: Thyroid adenomas, atrophy of normal thyroid, left ventricular hypertrophy, glomerulosclerosis with similar vascular lesions (not included).
Contributors Comment: This particular patient had multiple risk factors for developing hypertensive retinopathy and hyphema. A combination of thyroid-induced ventricular enlargement and renal failure, along with irregular treatment of the condition, produced a cycle of worsening disease. Histologic lesions primarily involve retinal and choroidal vessels, as in this case, with lesions ranging from fibrinoid necrosis to multi-layered onion-skin layering of medial hypertrophy and adventitial fibrosis. The animal has severe separation of the retina from the choroid with choroidal hypertrophy and hemosiderosis. Given the severity of retinal atrophy, it is likely that the cat had been blind for several weeks before hyphema was noticed clinically.
Intraocular hemorrhage is a frequent sequelum of high blood pressure in old cats.2,5 Renal disease, hyperthyroidism and cardiac disease are commonly contributory (this cat had a trifecta). Disease is usually symmetrical but with qualitative differences between eyes. This cat also developed hyphema in the right eye, but intraocular pressure did not become elevated and no corneal ulcer was found. Hypertensive lesions can be found in the retina, choroid and rarely iris. Vascular lesions result in retinal and preretinal hemorrhage and edema; with retinal detachment because of effusion from leaky choroidal vessels. Exudative retinal separation and retinal necrosis produce atrophy of the photoreceptive and characteristic tombstoning of the retinal pigment epithelium. In this eye intraocular pressure was increased, resulting in secondary open angle glaucoma.
The earliest retinal changes in hypertension are arteriolar narrowing secondary to vasospasm, followed by diffuse or focal narrowing of arteriolar walls, changes that can be seen on ocular exam. In progressive disease, the blood-retinal barrier breaks down, leading to fluid leakage, bleeding and ischemia of the nerve fiber layer. Severe disease in people portends an increased risk of cardiovascular mortality.1
Hyphema or hemorrhage into the anterior chamber results from disruption of the blood ocular barrier, and has a number of causes, including trauma, vessel-rich neoplasms and coagulopathy. In some of these conditions, only one eye is affected. Common sequelae include cataracts, glaucoma, synechiae, corneal staining by hemoglobin, and eventual phthisis. Other organs, including brain, heart and kidneys are common targets of hypertension. Bleeds due to hypertension can produce clotted or unclotted blood. Use of ultrasound can be useful, if blood obscures evaluation of the back of the eye. Persistent slow bleeding and alteration of intraocular structures suggests a poor prognsis.4
Decreased blood flow through the vasa vasorum during hypertension results in acute hypoxia and aortic medial necrosis. In turn, decreased flow results in increased vascular tone, neovascularization, leading to reduced vasodilatory capacity, creating a self-perpetuating cycle. Kidney disease, hyperthyroidism, hyperaldosteronism, anemia and diabetes are predisposing systemic diseases. Some studies indicate that arteriosclerosis is uncommon in normotensive cats. Remodeling of small arteries and arterioles results in narrow lumen diameter and hypertrophic remodeling of the media.3
JPC Diagnosis: Eye: Arteriolosclerosis, multifocal, moderate with severe intraocular hemorrhage, retinal atrophy and detachment, Domestic shorthair, feline.
Conference Comment: This case provided exceptionally descriptive microscopic lesions. Intraocular hemorrhage was the most prominent microscopic finding among conference participants. There was dialogue about the top four rule outs for hemorrhage in all chambers of the eye:
(1) Trauma (often a diagnosis of exclusion)
(2) Hypertensive retinopathy
(3) Neoplasia which can rupture and hemorrhage into the eye
(4) Inflammation especially due to hematogenous uveal localization of infectious agents
(5) Coagulopathy
It was obvious amongst conference participants that neoplasia and inflammation could be ruled out. However, since participants were not provided the clinical history in this case, a conversation ensued regarding how to separate trauma from hypertension microscopically.
Vascular changes are the best way to differentiate hypertension from trauma. With systemic hypertension, there is fibrinoid necrosis of the tunica media, thickening of arteriolar walls, narrowing of the vascular lumen most likely secondary to vessel damage and leakage of blood proteins into the wall which is best seen in the choroid and retinal vessels.6 The thickened walls and characteristic onion-skinned appearance were highlighted in this case with a periodic acid-Schiff stain. Based on our microscopic findings, we concur with the contributors diagnosis of hypertensive retinopathy and discussed the clinical findings in this case (described above) to include the associations of renal failure and hypertension/elevated intraocular pressure.
Renal disease is the most common cause of hypertension in dogs and cats and may either be a cause or an effect of hypertension. In either case, hypertension is self-perpetuating because medial hypertrophy and hyalinization of renal arteries lead to progressive nephrosclerosis, heightened hypertension, and increased pressure-induced damage in affected tissues.4 In this case, it is not clear which was the initial development: hyperthyroidism, renal disease, or hypertrophic cardiomyopathy. However, it is likely that all three contributed to the clinical and microscopic findings in this case.
Additionally, conference participants viewed several iridal changes, resulting in discussion of the following entities (not all present in this slide): anterior synechia (adherence of the iris to the cornea with compression of the drainage angle), posterior synechia (adherence of the iris to the lens), iris bombé (posterior synechia that involves the entire circumference of the iris and blocks flow of aqueous causing increased pressure in the posterior chamber and causing bowing of the iris forward), ectropion uveae (contraction of a pre-iridal fibrovascular membrane resulting in infolding of the pupillary border to adhere to the anterior iris surface), and entropion uveae (contraction of a pre-iridal fibrovascular membrane resulting in infolding of the pupillary border to adhere to the posterior iris surface).6
Contributing Institution:
Veterinary Medical Diagnostic Lab and Department of Veterinary Pathobiology
References:
1. DellaCroce JT, Vitale AT. Hypertension and the eye. Curr Opin Ophthalmology 2008;19:471-498.
2. Dubielzig RR, Ketring KL, McLellan GJ, Albert DM eds. Veterinary Ocular Pathology: a Comparative Review. Saunders-Elsevier: St Louis MO. 2010: 5, 370-372.
3. Kohnken R, Scansen BA, Premanandan C. Vasa vasorum arteriopathy: relationship with systemic arterial hypertension and other vascular lesions in cats. Veterinary Pathology.2016. epub doi: 10.1177/0300985816685137.
4. Robinson WF, Robinson NA. Cardiovascular system. In Maxie G, ed. Jubb, Kennedy, and Palmers Pathology of Domestic Animals Vol 3, 6th ed. Elsevier, Inc. St. Louis; 2016:59-60.
5. Telle MR, Betbeze C. Hyphema: considerations in the small animal patient. Topics Copan Anim Med 2015;30:97-106.
6. Wilcock BP, Njaa BL. Special senses. In Maxie G, ed. Jubb, Kennedy, and Palmers Pathology of Domestic Animals Vol 1, 6th ed. Elsevier, Inc. St. Louis; 2016:447-449, 472-473.