Signalment:
On presentation, the patient's mucus membranes were cyanotic, pulse = 162, respiratory rate = 60 - 80, and crackles were ausculted bilaterally. No murmur was heard, but heart sounds were difficult to hear over the crackles. The dog was placed in an oxygen cage and heart rate decreased to 120 and mucus membranes were pink. Jugular pulses were increased. Cough could not be elicited on tracheal palpation. Respiratory rate and effort remained increased while in the oxygen cage.
Only one lateral thoracic radiograph was able to be obtained before the dog became very distressed and was placed back in the oxygen cage. The radiograph showed mild to moderate right sided cardiomegally and diffuse interstitial to alveolar lung pattern, more pronounced dorsocaudally.
A brief echocardiogram, with the dog standing in the oxygen cage, revealed extremely enlarged right ventricle with thickened free wall.
Physical exam, radiographic and echocardiographic studies were all consistent with pulmonary fibrosis and pulmonary hypertension.
Gross Description:
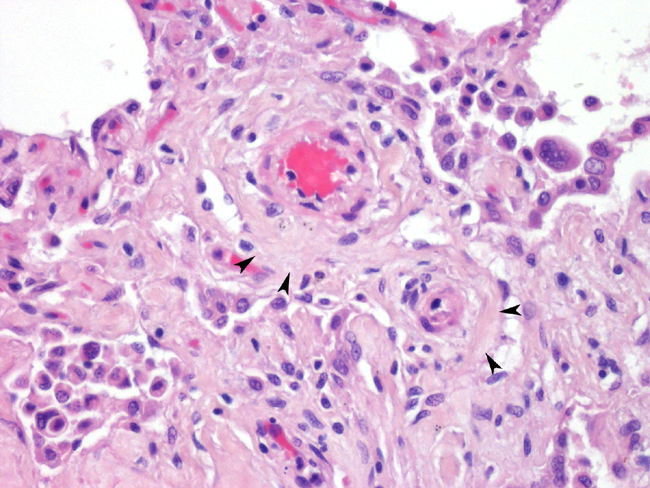
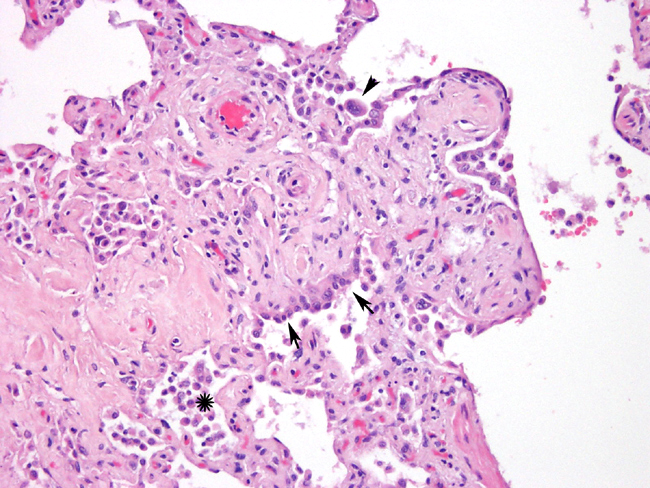
Histopathologic Description:
Masson's trichrome stain shows moderate diffuse staining of the alveolar septae. There is multifocal to diffuse staining of cells within the alveolar septae for smooth muscle actin (myofibroblasts). There is negative staining for Collagen type I. (Reliable immunostains for collagen III, and IV were unavailable). Many intraalveolar cells stain positive for cytokeratin (pneumocytes).
Morphologic Diagnosis:
Lab Results:
Leukocytosis (23.5000 x103/ul; reference range 4.900 - 16.900 x103/ul) with mature neutrophilia (19.270 x103/ul; reference range 2.800 - 11.500 x103/ul). No abnormalities were noted on the differential. Alkaline Phosphatase was markedly increased (1484 U/L; reference range 12 - 121 U/L)
Condition:
Contributor Comment:
Histopathologic findings consistently show generalized thickening of the interstitium by variable amounts of eosinophilic extracellular matrix. The process can range from diffuse to multifocal or regional. The most severe cases have multifocal areas of type II pneumocyte hyperplasia. There are often variable amounts of inflammatory cells (lymphocytes, plasma cells, macrophages.) Masson's trichrome stains the extracellular matrix expanding the alveolar septae as collagen1. Immunohistochemistry reveals that there can be a mixture of type I and type III collagen depending on the severity and chronicity of the disease1. Ultrastructurally, the extracellular matrix consists of numerous bundles of electron dense fibrils aligned parallel to one another. Individual fibrils have even spaced band periodicities (collagen)1.
Differentials for idiopathic interstitial lung disease include, chronic bronchiolitis, neoplasia, and infectious diseases5. Idiopathic interstitial lung disease is of unknown etiology. Infectious processes, drug reactions, exposure to toxins or dust, and connective tissue disorders have been hypothesized as potential etiologies. Diagnosis, treatment, and determining an underlying etiology is difficult because by the time clinical signs are seen, there is usually irreversible loss of pulmonary function (fibrosis), and the inciting cause may no longer be present.Â
In human medicine there are a group of idiopathic pneumonias with similar features of shortness of breath, radiographic evidence of diffuse pulmonary infiltrates and varying degrees of inflammation, and fibrosis. The terminology in human medicine for these diseases has changed. Previously, many form of idiopathic interstitial pneumonia were termed "idiopathic pulmonary fibrosis", which is now reserved for a specific type also known as "usual interstitial pneumonia" or "cryptogenic pulmonary fibrosis"3. This diseasae in humans has some similarities as the disease seen in West highland White terriers but technically the same. Other types of idiopathic interstitial pneumonias besides usual interstitial pneumonia, include, acute interstitial pneumonia, non-specific interstitial pneumonia, cryptogenic organizing pneumonia, and desquamative interstitial pneumonia-respiratory bronchiolitis interstitial lung disease3.
JPC Diagnosis:
Conference Comment:
Additional causes of pulmonary fibrosis were discussed. Anything that damages type I pneumocytes or alveolar endothelium may lead to pulmonary fibrosis. Causes of alveolar damage include irradiation, septicemia, thermal injury, vomit aspiration, toxic gases (e.g., oxygen toxicity) and toxins (e.g., paraquat).
Other conditions with an increased prevalence in West Highland White Terriers include craniomandibular osteopathy, polycystic liver and kidney disease, hyperplastic dermatosis, and chronic hepatitis and cirrhosis.
References:
2 Corcoran BM, Cobb M, Martin MWS, Dukes-McEwan J, French A, Fuentes VL: Chronic pulmonary disease in West Highland White Terriers. Vet Rec 144:611-616, 1999
3. Gross TJ, Hunninghake GW: Idiopathic pulmonary fibrosis. N Engl J Med 345:517- 525, 2001
4. Lobetti RG, Milner R, Lane E: Chronic idiopathic pulmonary fibrosis in five dogs. J Am Anim Hosp Assoc 37:119-127, 2001
5. Webb JA, Armstrong J: Chronic idiopathic pulmonary fibrosis in a West Highland white terrier. Can Vet J 43:703-705, 2002