Wednesday Slide Conference, Conference 1, Case 3
Signalment:
7 years of age, female, Selle Français, Equus caballus, Horse.
History:
The mare was initially presented to the referral clinic due to symptoms of chronic, recurrent diarrhea and intermittent exercise intolerance. General clinical examination revealed no abnormalities, with the exception of an enlarged, non-painful, retropharyngeal lymph node on the left side. Hematology, basic blood chemistry, and parasitological examination were normal. The horse was sent home after oral treatment with prednisolone (Equisolon®).
1 month later the horse suffered from severe, acute, right-sided epistaxis and was re-admitted to the clinic and hospitalized. Endoscopy of the upper airways revealed the presence of large amounts of blood in pharynx and trachea, as well as a large blood clot filling the lumen of the right guttural pouch. The left guttural pouch was evaluated as normal.
Surgery under general anesthesia was performed with fluoroscopy-guided placement of 7 intra-arterial coils in carotid and maxillary arteries. During recovery excitation and epistaxis developed. An emergency ligation of the right-sided a. carotis communis was attempted but proved ineffective. The horse was subsequently euthanized.
Gross Pathology:
The right guttural pouch was filled with clotted blood and contained a sharply delineated slightly raised irregular white plaque ca. 6 cm in diameter (suggestive of mycosis) at the level of the medial wall, with several smaller blood clots adherent to this area. Which, when removed, revealed a focal depression in the wall and a frayed transmural defect of a large thick-walled blood vessel (a. carotis interna).
The left side guttural pouch did not contain any blood but a smaller, ca. 4 cm diameter, pale plaque was found adherent to the wall.
Other significant gross findings included pale oral mucosae, blood exuding from both nostrils, and hemorrhagic contents of stomach and duodenum.
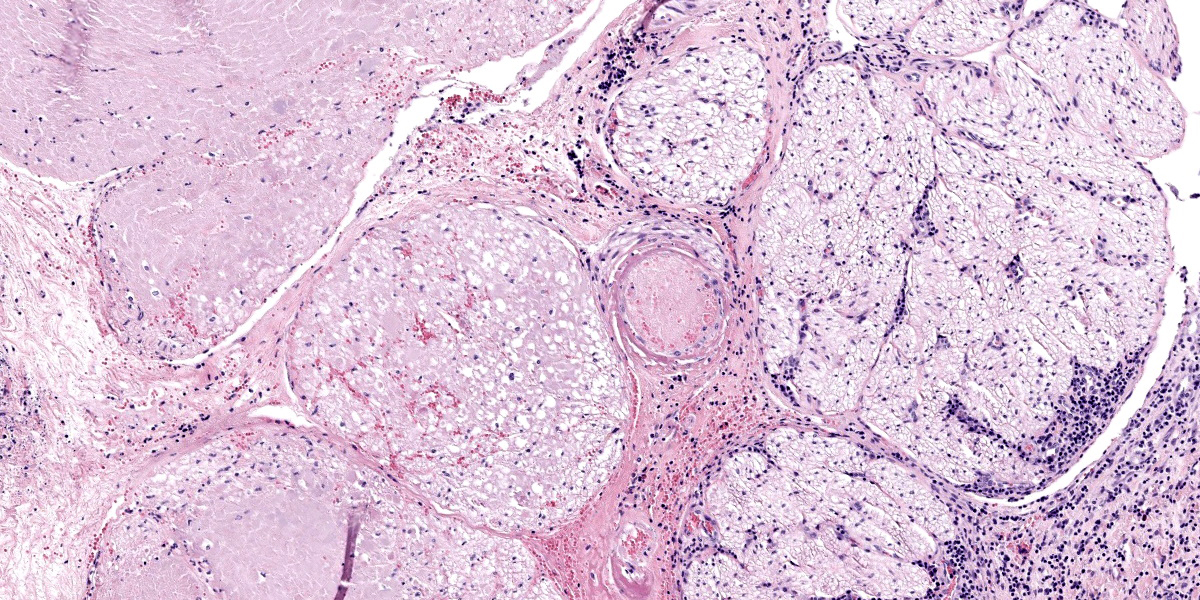
Microscopic Description:
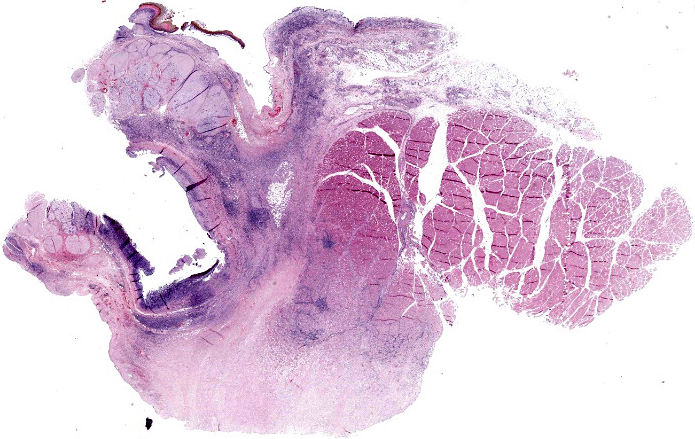
Guttural pouch, part of large vessel wall, associated nerves and muscle.
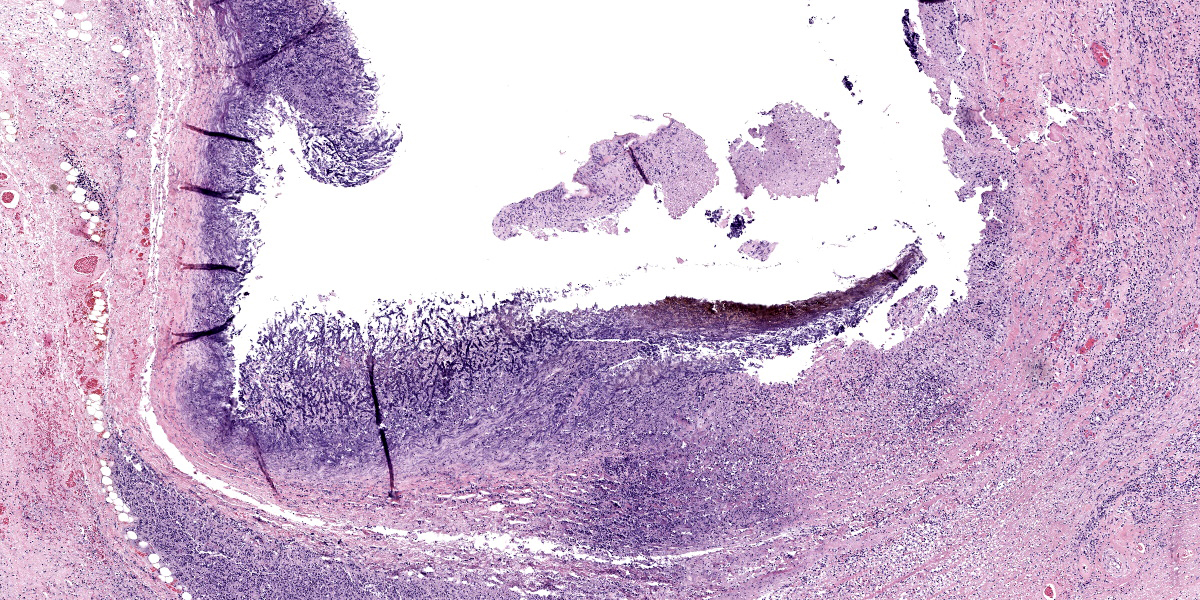
The endothelium of the large artery is multifocally eroded and replaced by a layer of fibrin, admixed with erythrocytes (hemorrhage), eosinophilic necrotic cell and nuclear debris, and few partially degenerate neutrophils (arteritis).
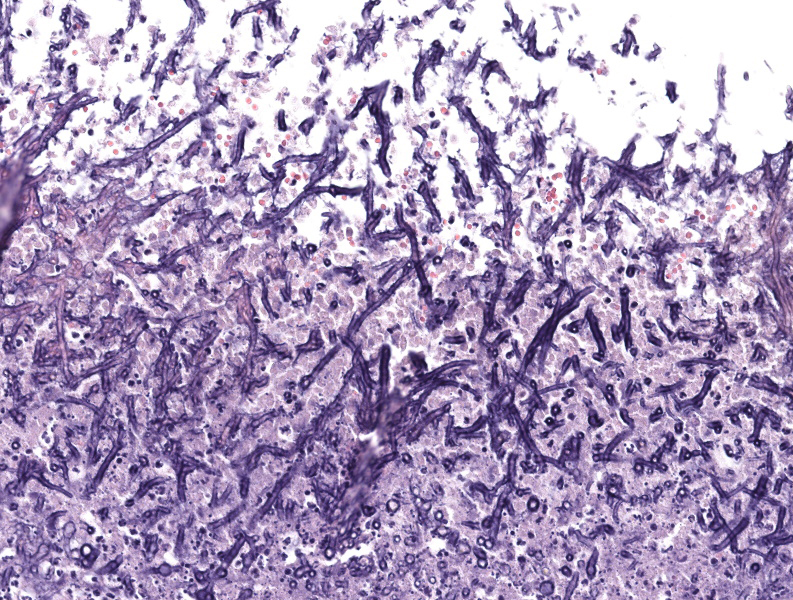
At the level of the eroded surface and penetrating deeper into the tunica media and connective tissues a moderate amount of ca. 5-8µm long deeply basophilic structures with parallel walls can be found, sometimes seen to be dichotomously branching, and often endospore-forming (fungal hyphae). The severity of the arteritis and presence of hyphae is dependent on the level of tissue section.
Smaller vessels show hyalinization of the wall and contain mixed nuclear dust and a dense infiltration of neutrophils (thrombosis and vasculitis).
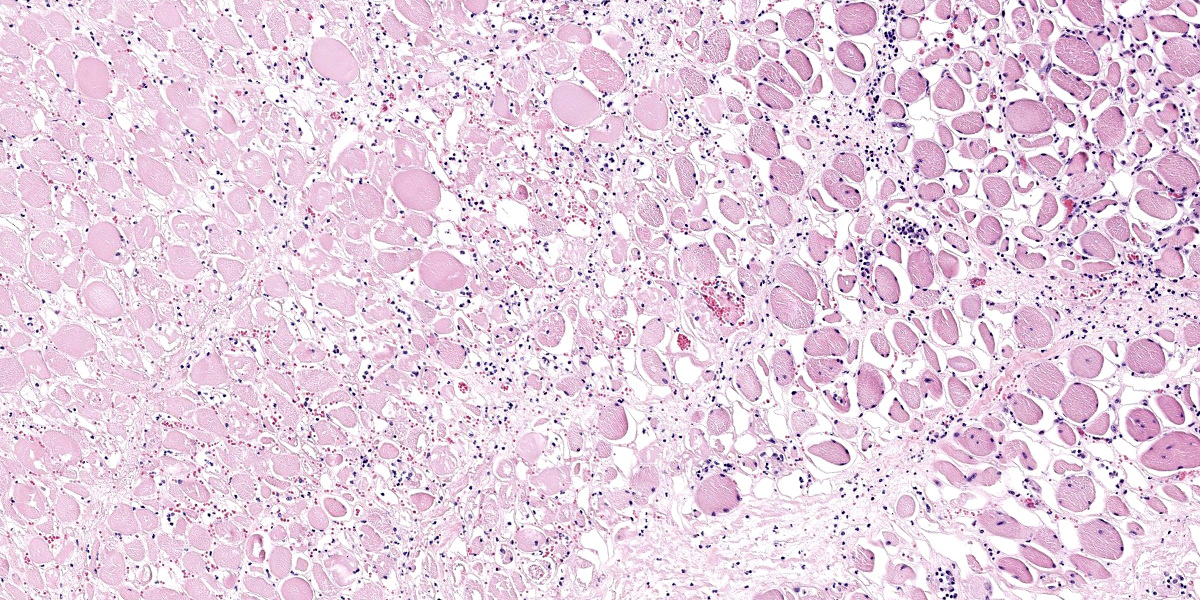
Multifocal areas of coagulative necrosis surround and infiltrate muscle fibers and nerve fibers deep in the tissue, along with the presence of occasional fungal hyphae.
Contributor’s Morphologic Diagnosis:
Mycotic air sacculitis, chronic, severe, erosive, necrotizing, with intra-lesional fungal hyphae, obliterating necrosuppurative arteritis, multifocal vascular thromboses, and local necrotizing fungal myositis and neuritis.
Contributor’s Comment:
The equine guttural pouches are a somewhat unique bilaterally symmetrical anatomical structure which can be interpreted as a local diverticulum of the inner auditory tube or Eustachian tube in which several important structures can be found.10 It is longitudinally divided into two communicating compartments, lateral and medial, by the stylohyoid bone. Their functionality has been a topic of discussion for many decades or even centuries, but Ninomiya & Kuwano confirmed them to play a role as an effective countercurrent heat exchanger cooling arterial blood flowing towards the brain.10
Equine guttural pouch mycosis is a rare but potentially highly morbid and possibly fatal disease, most often caused by Aspergillus spp. in temperate climates, which are fairly ubiquitous opportunistic pathogens present in upper airways of healthy equids as well as in their immediate surroundings.3,4,5,6,8
There appears to be no predilection in regard to breed, sex, age, or left versus right side air sacs.3 The fungal hyphae, especially of A. fumigatus, are typically angiotropic/angioinvasive and therefore often form infiltrative mycotic plaques associated with the large blood vessels lying closely beneath the guttural pouch surfaces.1,8,5
It can be considered challenging to diagnose, in part due to the wide spectrum of possible clinical signs, but also due to the high risks associated with confirmation of the pathogen in situ.7,11 In this particular case, based on the history, gross lesions, and microscopic findings, infection with Aspergillus spp. was found to be most likely, though the presence of other non-pigmented hyphae producing fungi cannot be excluded.4
Contributing Institution:
Department of Pathology, Microbiology and Avian Diseases
Faculty of Veterinary Medicine, University of Ghent
Salisburylaan 133, 9820 Merelbeke, BELGIUM
veterinaire.pathologie@ugent.be
+ 32 9 264 77 41
https://www.ugent.be/di/di05/nl
JPC Diagnosis:
Guttural pouch: Eustachitis and arteritis, necrotizing, chronic, diffuse, severe, with numerous fungal hyphae, fibrin thrombi, and infarction of skeletal muscle and nerves.
JPC Comment:
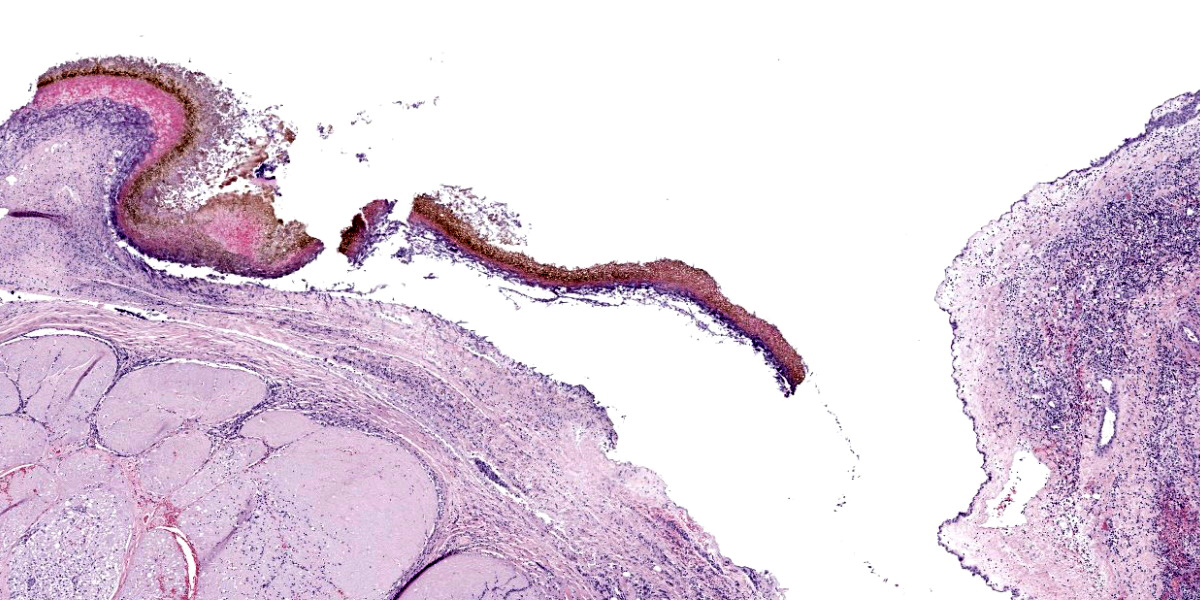
The exact tissue identification for Case 3 is subtle, though the presence of a large blood vessel next to nerves, deeper muscle and a thin layer of squamous epithelium is suggestive of the equine guttural pouch (figure 1-1). That stated, the magnificent fungal arteritis that the contributor has shared with us quickly pares down the differential list. Like the previous case, fungal elements are also a major diagnostic feature though the distribution and tissue response is quite different from Case 2. GMS and PAS stains were less remarkable for this case, though this may simply reflect luck and plane of section for the slides we selected. Conference participants felt that the features on H&E were highly suggestive of Aspergillus, though they did remark on the pigmentation present along the guttural pouch mucosa and whether this might be related to another fungal species instead (figure 3-7).
As the contributor notes, guttural pouch mycosis is often caused by Aspergillus species and the large fungal mats along the surface of and expanding into large blood vessels is a helpful diagnostic feature.2 While hemorrhage and epistaxis are common clinical manifestations of guttural pouch mycosis, they are not the only significant ones to consider. Marked guttural pouch inflammation can extend into adjacent structures to include the vagosympathetic trunk, bones , middle ear, brain, or joints.2 Dysphagia, Horner’s syndrome, and laryngeal hemiparesis have all been reported secondary to guttural pouch mycosis.2 Although the animal in the present case did not have reported neurologic deficits at the time of euthanasia, there is marked necrotizing arteritis that spills over to adjacent skeletal muscle (myositis) and nerves (neuritis) quite spectacularly. For a similar case from the WSC archives, check out, see Conference 21, Case 2, 2012-2013.
Other diseases of the guttural pouch to consider include guttural pouch tympany, guttural pouch empyema, temporohyoid osteoarthropathy, and neoplasia.2,11 Tympany is uncommon and is seen in young horses secondary to congenital conformational abnormalities or inflammation that leads to retention of air and expansion of the guttural pouch. Empyema is seen secondary to respiratory infection, most commonly Streptococcus equi, and purulent nasal discharge (not hemorrhage) is the typical finding. Neoplasia of the guttural pouch is rare, but squamous cell carcinoma has been reported.2 Temporohyoid osteoarthropathy reflects remodeling of either/both the stylohyoid bone and petrous temporal bone; this may occur secondary to otitis media, respiratory infection, or degenerative conditions.11 Diagnostic imaging, to include, radiography, endoscopy, and computed tomography are helpful at distinguishing these diseases amid a complex anatomical landscape. 11
References:
- Brandão ISL, Oliveira-Moraes H, Souza Motta CM, Oliveira NTD, Magalhães O. Elastin increases biofilm and extracellular matrix production of Aspergillus fumigatus. Brazilian Journal of Microbiology. 2018; 49: 675–682.
- Caswell JL, Williams KJ. Respiratory System. In: Maxie MG, ed. Jubb, Kennedy & Palmer's Pathology of Domestic Animals. Vol 2. 6th ed. St. Louis, MO: Elsevier; 2016:480-481.
- Dobesova O, Schwarz B, Velde K, Jahn P, Zert Z, Bezdekova B. Guttural pouch mycosis in horses: a retrospective study of 28 cases. Veterinary Record. 2012; 171: 561-561.
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clinical Microbiology Reviews. 2011; 24: 247-280.
- Kipar A, Frese K. Hypoglossal neuritis with associated lingual hemiplegia secondary to guttural pouch mycosis. Veterinary Pathology. 1993; 30: 574-576.
- Lepage OM, Perron MF, Cadoré JL. The mystery of fungal infection in the guttural pouches. The Veterinary Journal. 2004; 168: 60-64.
- Lepage OM. Challenges associated with the diagnosis and management of guttural pouch epistaxis in equids. Equine Veterinary Education. 2016; 28: 372-378.
- Ludwig A, Gatineau S, Reynaud MC, Cadoré JL, Bourdoiseau G. Fungal isolation and identification in 21 cases of guttural pouch mycosis in horses (1998–2002). The Veterinary Journal. 2005; 169: 457-461.
- Nadkarni T, Goel A. Aspergilloma of the brain: an overview. Journal of Postgraduate Medicine. 2005; 51: 37-41.
- Ninomiya H, Kuwano A. Microvasculature of the Guttural Pouch Mucosa and Relationship With the Internal Carotid Artery in Horses. Journal of Equine Veterinary Science. 2019; 74: 84-89.
- Pollock PJ. Diagnosis and management of guttural pouch mycosis. Equine Veterinary Education. 2007; 19: 522-527.
- Thomas-Cancian A, Ségard-Weisse E, Drumond B, Cadoré J-L. Diagnostic Imaging of Diseases Affecting the Guttural Pouch. Veterinary Sciences. 2023; 10(8):525.