Signalment:
Nine-year-old castrated male Labrador
retriever (
Canis familiaris).Right pelvic
limb swelling noticed in July 2012. Treated with prednisone, diphenhydramine,
cephalexin. Viscous fluid aspirate from limb 8/8/12. Presented to Internal
Medicine 9/4/12 - chest x-rays unremarkable, right pelvic limb x-rays showed an
aggressive lesion involving distal femur, with soft tissue swelling involving
down to distal tibia. Aspiration cytology - probable sarcoma.
Abdominal
ultrasound and pelvic CT scan showed a large cystic mass involving the right
pelvic limb with bone invasion and presumed metastasis to the right inguinal
and right medial iliac lymph node. Possible femoral vein thrombus. High
coxofemoral disarticulation amputation performed. Clinical diagnosis: Sarcoma
with lymph node metastasis.
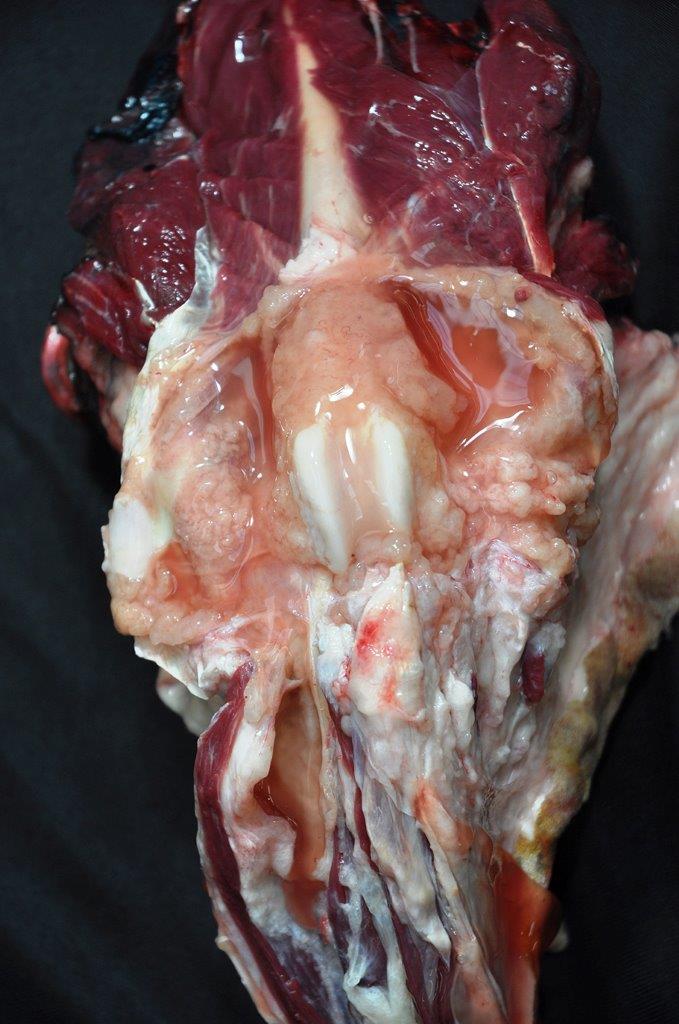
Gross Description:
A
right pelvic limb from the femoral head and distally was submitted. The stifle
joint and muscles of the thigh were expanded by palpably viscous, coalescing
nodules. The popliteal lymph node was bi-lobed and measured approximately 2.6 x
1.4 x 1 cm. On cut surface, was mottled dull yellow, red to red-brown, slightly
bulging and contained multifocal to coalescing round to oval, 0.2-0.5cm, soft
to firm cystic structures filled alternatively with small amounts of clear,
colorless fluid to opaque, firm, off-white material. On cut surface, the stifle
joint was expanded by a 5x6x5cm, mottled dull yellow, red to red-brown,
slightly bulging mass of multifocal to coalescing round to oval, soft to firm
cyst-like structures that were filled alternatively with small amounts of
clear, colorless fluid to opaque, firm, off-white material. Large amounts of
mucoid, gelatinous, dull, yellow-red material expanded fascial planes,
lymphatic vessels, and subcutaneous tissues from the mid-femur distally, and
most severely, along the proximal and mid-tibia. The stifle joint was expanded
by approximately 40 ml of the same
material. The synovium of the stifle joint was diffusely thickened with
papillary and ovoid projections and cavitations as previously described in the
popliteal lymph node. The joint capsule as variably friable to firm. The entire
limb was sagittally sectioned and on cut surface a firm to soft mass composed
of thousands of small, firm, semi-transparent, off-white nodules emanated from
the plantar aspect of the level of the stifle joint. The mass com-pressed the
normal structures of the region. Approximately 3-5 small (0.8x0.5cm), ovoid,
firm, semi-translucent, off-white masses tracked along and were adhered the
femoral vasculature adventitia, including approximately 1.0cm from the surgical
margin.
The
inguinal lymph node was also submitted and measured 6 x 3.5 x 1.8 cm and on cut
surface is expanded by multilobulated, multicavitated nodules that vary in size
from 0.9 cm to 1.3 cm in diameter. They are round to oval and contain variable
amounts of mucoid, tenacious, clear, colorless fluid.
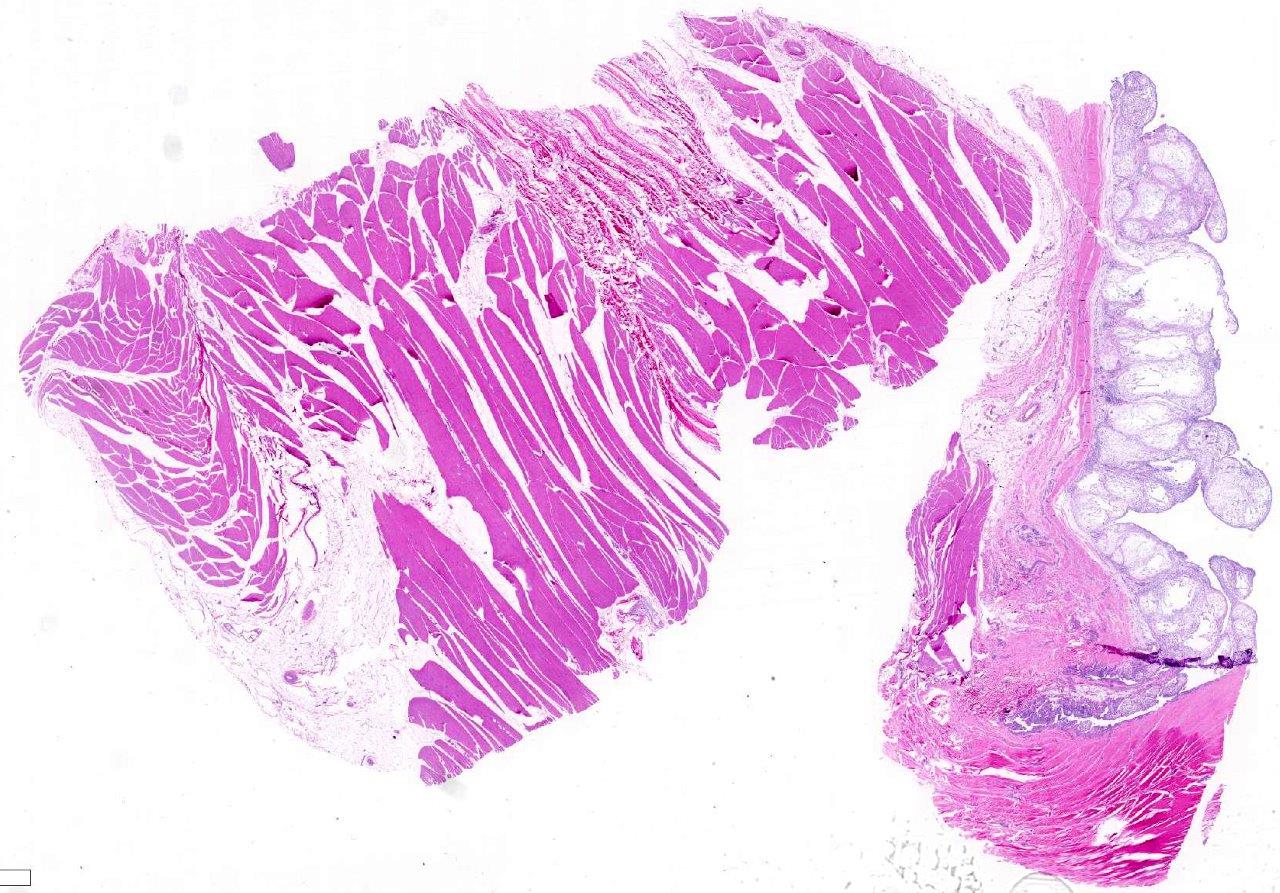
Histopathologic Description:
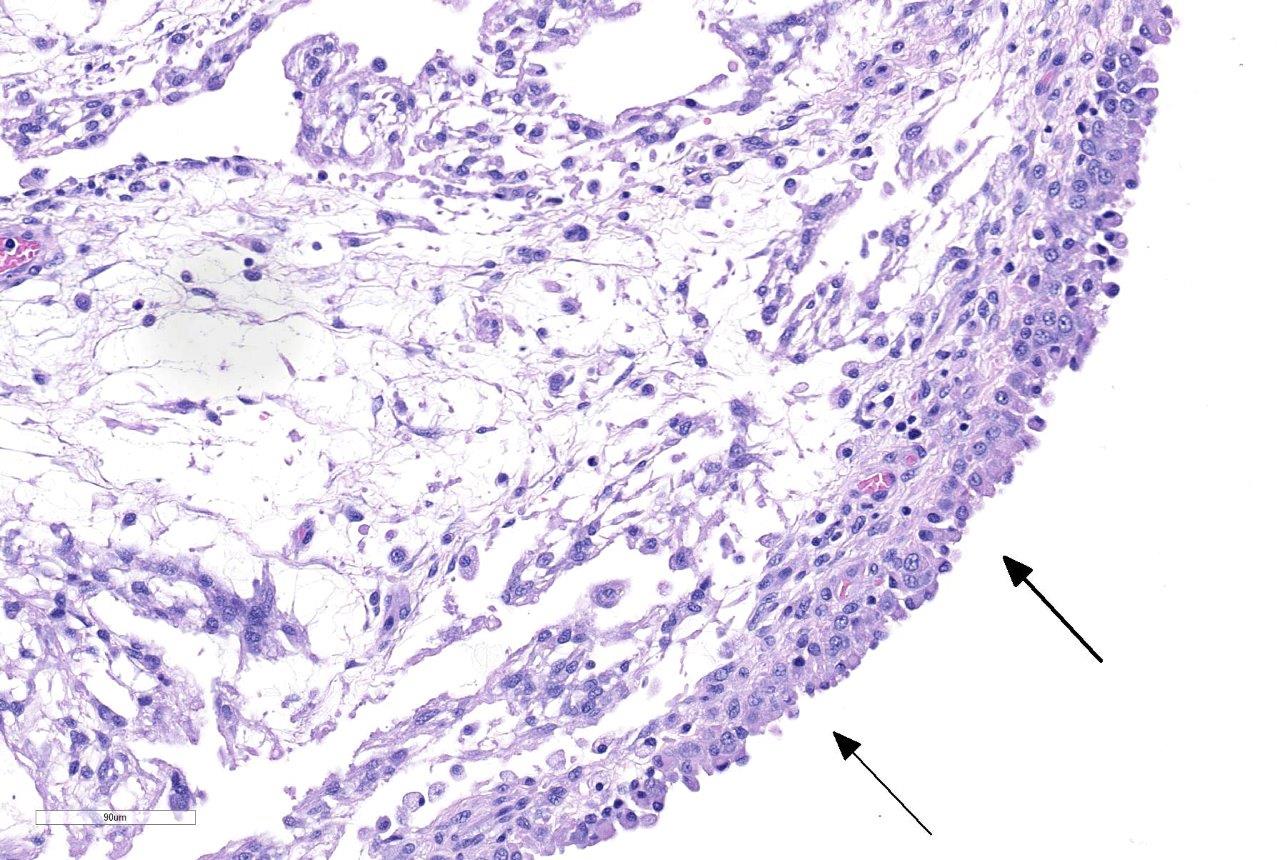
Examined
are two cross sections of joint capsule which are markedly thickened up to 0.9
cm by a poorly cellular, abundantly myxoid, multinodular, unencapsulated,
expansile neoplastic mass that primarily occupies the subintimal space.
Individual variably-sized nodules are separated by thin bands of fibrous
connective tissue. The neoplastic nodules often merge and are comprised of
abundant amounts of lacy, gelatinous, pale, amphophilic to basophilic matrix
and widely spaced stellate to spindloid cells. The cells are cytologically
bland, have ill-defined borders and small amounts of a finely granular,
eosinophilic cytoplasm. Nuclei are oval, with granular chromatin and variable
numbers of ill-defined nucleoli. Aniso-cytosis and anisokaryosis are mild. No
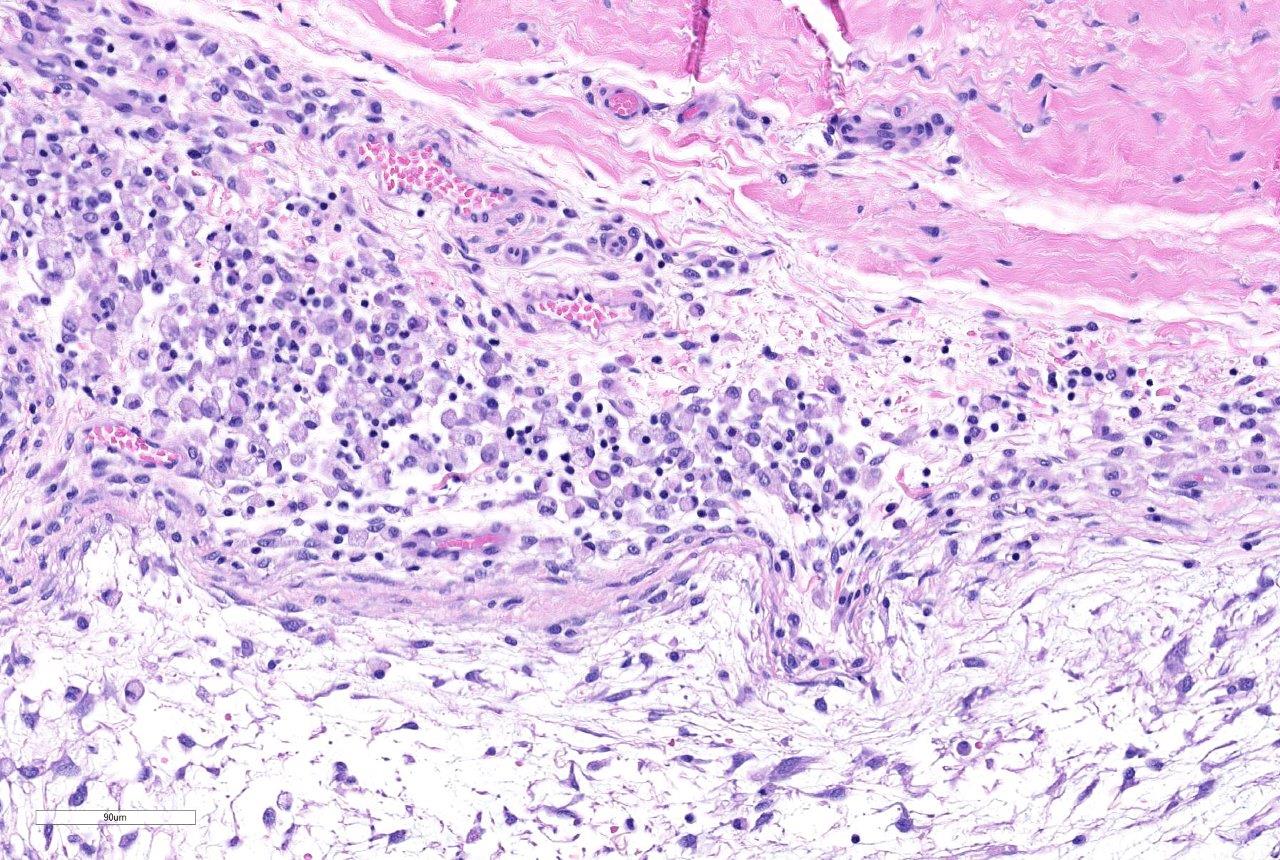
mitotic figures are observed. Multifocally along the most superficial aspects
of the subintima, deep to synoviocytes, there are moderate to large numbers of
lymphocytes and fewer plasma cells. Rarely, pigment-laden cells (macrophages)
admix with the lymphocytes and plasma cells. The intimal layer is multifocally
hyperplastic and jumbled up to 10 layers. The fibrous capsule is expanded by
abundant fibrovascular tissue, adipose, and multifocal aggregates of plasma
cells, lymphocytes, and fewer mast cells.
Morphologic Diagnosis:
Femorotibial (Stifle) Joint and
associated skeletal muscle, Right Popliteal and Inguinal Lymph Nodes: Synovial
myxoma with local invasion and multiple lymph node metastases.
Lab Results:
Radiographic findings: There is marked soft tissue swelling
surrounding the tibia and loss of the normal fascial plane distinction. There
are lobular soft tissue densities at the medial aspect of the right stifle
joint. There is permeative lysis of the distal femur, resulting in a coarse
trabecular pattern and sclerosis with an indistinct transition zone between
normal and abnormal bone. Periarticular osteo-phytes are present on the apex of
the patella, the fabellae, the proximal tibia, and the distal femur. There is
marked increased soft tissue opacity associated with the stifle joint.
Radiographic
Impressions: Aggressive bone lesion affecting the distal right femur with
adjacent lobular soft tissue opacities is concerning for a soft tissue neoplasm
with extension to the bone such as a synovial cell sarcoma. Mild secondary
joint disease. Marked edema of the right crus. An ultrasound examination of the
right stifle is recommended if clinically indicated. Pulmonary osteomas. No
radiographic evidence of pulmonary metastatic disease.
CT
Scanning impressions: Large cystic right pelvic limb mass with associated sub-cutaneous
edema and bone invasion. Filling defect of the right femoral vein may be
secondary to tumor invasion or thrombus formation. Metastatic inguinal and sub-lumbar
lymph nodes. The appearance of the right hypogastric and mesenteric lymph nodes
may represent metastases or reactivity.
Cytology
of stifle mass: Four moderately cellular coverslips are examined that have a
medium pink stippled background and a mild amount of blood with erythrocytes
frequently distributed in a prominent windrowing pattern. Nucleated cells are
distributed individually and in variably sized loose aggregates. Thick pink
fibrillar material is frequently seen associated with cell aggregates.
Individual cells consist predominantly of macrophages / synoviocytes. Cells in
clusters have a low to moderate amount of pale cytoplasm that frequently causes
polar wisps giving the cells a spindloid shape. Nuclei are ovoid with coarsely
stippled chromatin and small nucleoli. Low numbers of small mature lymphocytes
are also noted.
Cytologic
interpretation and comments: Probably sarcoma. The large aggregates of
spindloid shape cells are consistent with a sarcoma, with considerations
including spindle cell sarcoma, synovial sarcoma or even atypical
chondrosarcoma, however, this is considered less likely.
Condition:
Synovial myxoma
Contributor Comment:
Histiocytic
sarcoma, synovial sarcoma, and synovial myxoma are three differentials for
canine primary joint tumors.
2,3 All can cross joints and cause bony
lysis and proliferation. Synovial myxoma occurs uncommonly in dogs and is
widely considered to be a benign, but infiltrative, tumor of the joint.
Numerous cases of lymph node metastases, however, have been observed
(Contributing Institution experience). The stifle and digital joints are most
commonly affected. The three types of cells in synovial membranes are Type A
synoviocytes (macro-phage/dendritic cell origin), type B (fibroblast-like), and
type C (transitional, hematopoietic, or stem cell-like). Although a joint
tumor, the cell of origin of synovial myxomas is unknown; this is reflected in
the non-specific immunohistochemistry (IHC). They are vimentin positive.
Approximately 20-40% of synovial myxoma cells are CD18 immunoreactive and are
morphologically indistinguishable from CD18 negative joint cells. Synovial
myxomas are cadherin 11 and HSP25 immunoreactive, much like synovial cell
sarcomas and histiocytic sarcomas.
3 The most striking histologic
feature of synovial myxomas is the sparse, stellate to spindle cells that
elaborate abundant, coalescing nodules of myxo-matous matrix.
2,3,5
Again, although cytomorphologic features are generally bland, synovial myxomas
can metastasize to lymph nodes and be highly locally invasive.
2,3,5
JPC Diagnosis:
Joint,
stifle (per contributor): Synovial myxoma, Labrador retriever,
Canis
familiaris.
Conference Comment:
We thank the contributor for their institutions extensive
work-up on this case and excellent quality gross images. Of the three
differentials for canine joint neoplasms mentioned above, synovial myxoma is
the second most common neoplasm occurring within the joints of dogs, behind
histiocytic sarcoma and ahead of the rare synovial sarcoma (if such a tumor
truly exists.)
1,3,4 This neoplasm most commonly affects middle-aged
large breed dogs. Doberman pinschers and Labrador retrievers, as in this case,
are most often affected. It has also been rarely reported in cats.
1,4
Synovial myxomas usually affect a single joint, with the stifle and digit the
most commonly reported locations. These neoplasms are slow-growing and can
persist for months to years and often present as chronic lameness with or
without evidence of joint swelling.
1,3,4
Although
this is classified as a benign neoplasm, it can be locally infiltrative and
cause lytic lesions in the bone with significant articular lesions and
periarticular osteophyte formation. The conference moderator instructed that
radiographically, synovial myxoma cannot be reliably differentiated from
histiocytic sarcoma or synovial sarcoma.
3,4 Despite this locally
invasive behavior, the prognosis is typically good after complete surgical
excision. Bony lysis and infiltration usually necessitate amputation; however,
cases that lack bone lysis and extension outside of the joint capsule can be
treated with a simple synovectomy, which is curative in about 90% of reported
cases. In contrast, histiocytic sarcomas are associated with a poor prognosis,
with an average survival of just 5.3 months.
1,3,4 This significant
difference in biological behavior and prognosis highlights the importance of histopathology of the mass
prior to treatment. Interestingly, the conference moderator and highly regarded
veterinary pathologist with expertise in bone and joint pathology, Dr. Linden
Craig, remarked that this is the first example of a synovial myxoma she has
seen with metastasis. Given the observation by the contributors intuition of
multiple cases of lymph node metastasis for this neoplasm, Dr. Craig remarked
that the biological behavior of this neoplasm may need further review.
Conference
participants noted that once the tissue is identified as joint capsule with
adjacent skeletal muscle, the diagnosis of synovial myxoma is relatively
straight-forward. This neoplasm has a highly characteristic appearance of
variably sized nodules of stellate to spindle cells with long cytoplasmic
processes supported in a highly myxoid matrix and covered by a hyperplastic
synovial lining.
1,3,4 The conference moderator noted that the cell of
origin of synovial myxoma is not yet known; although, it is thought that given
the abundant myxoid matrix, the cell type is likely type B (fibroblastic)
synoviocytes. Type B synoviocytes normally produce hya-luronan, a large linear
glycosaminoglycan and major component of synovial fluid.
1,3,4
Despite this uncertainty of cell origin, the diagnosis can usually be made
without the aid of immuno-histochemical staining.
References:
- Craig LE, Ditmer
KE, Thompson KG. Bones and joints. In Maxie, MG, ed. Jubb, Kennedy,
and Palmers Pathology of Domestic Animals, Vol I. 6th ed.
Philadelphia, PA: Elsevier Ltd; 2016:159-162.
- Craig LE, Julian
ME, Ferracone JD. The diagnosis and prognosis of synovial tumors in dogs:
35 cases. Vet Pathol. 2002; 39(1):66-7.
- Craig LE, Krimer
PM, Cooley AJ. Canine synovial myxoma: 39 cases. Vet Pathol. 2010;
47(5):931-6.
- Craig LE, Thompson
KG. Tumors of joints. In: Meuten DJ ed. Tumors in Domestic Animals.
5th ed. Ames, IA: John Wiley and Sons Inc; 2017:337-350.
- Izawa T, Tanaka M,
Aoki M, Ohashi F, Yamate J, Kuwamura M. Incidental synovial myxoma with
extensive intermuscular infiltration in a dog. J Vet Med Sci. 2012;
74(12):1631-3.