Wednesday Slide Conference, Conference 1, Case 2
Signalment:
8-year-old, male castrated, Arabian horse (Equus ferus caballus).
History:
This is a mass surgically removed from the left thorax.
Gross Pathology:
N/A
Microscopic Description:
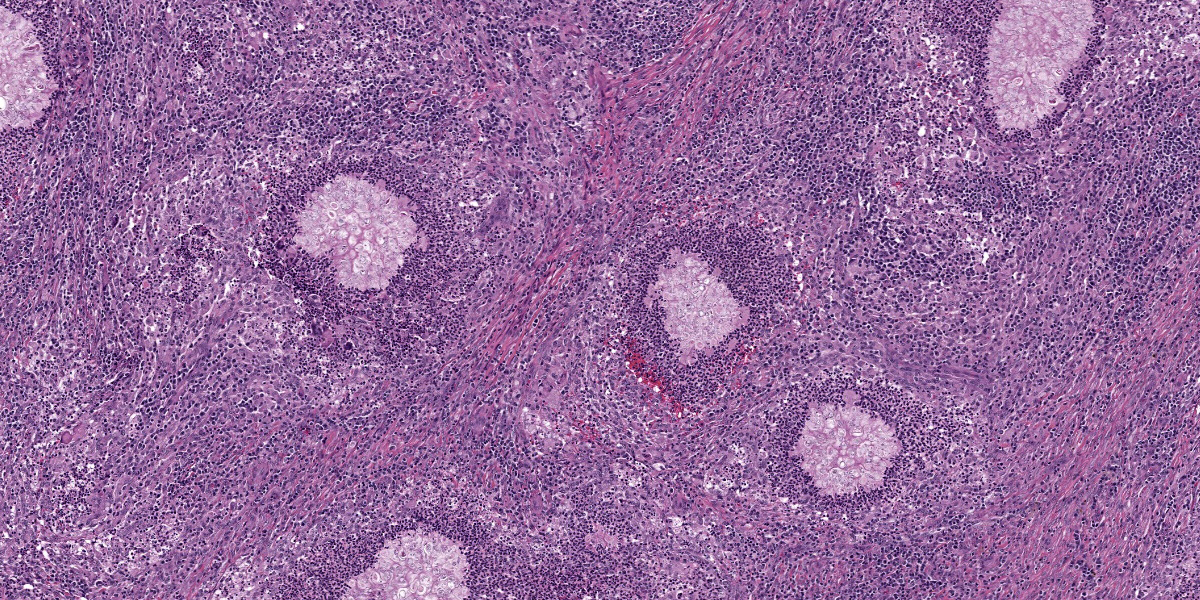
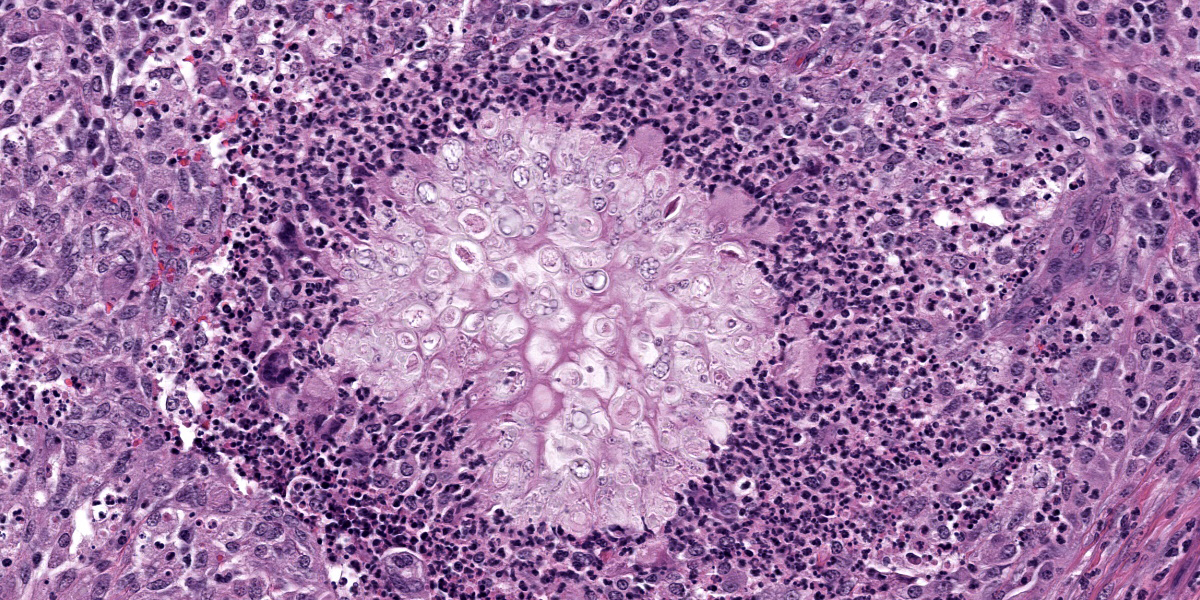
Subcutis (mass from the left thorax): Expanding the deep dermis and extending to the subcutis are numerous multifocal to coalescing pyogranulomas. The pyogranulomas are composed of intact and necrotic neutrophils surrounded by epithelioid macrophages, occasional multinucleated giant cells with up to 20 nuclei, fewer lymphocytes and plasma cells. In the center of the pyogranulomas are irregular pools of lightly eosinophilic amorphous material forming grain or granular structures measuring up to 500 um that contain countless tight clusters of polymorphic, refractile, fungal hyphae with frequent bulbous dilations. Surrounding the pyogranulomas are variably thick bands composed of fibroblasts and collagen (fibrosis). Multifocally, the surrounding dermis and subcutis are infiltrated by moderate numbers of lymphocytes and plasma cells, and rare macrophages and neutrophils.
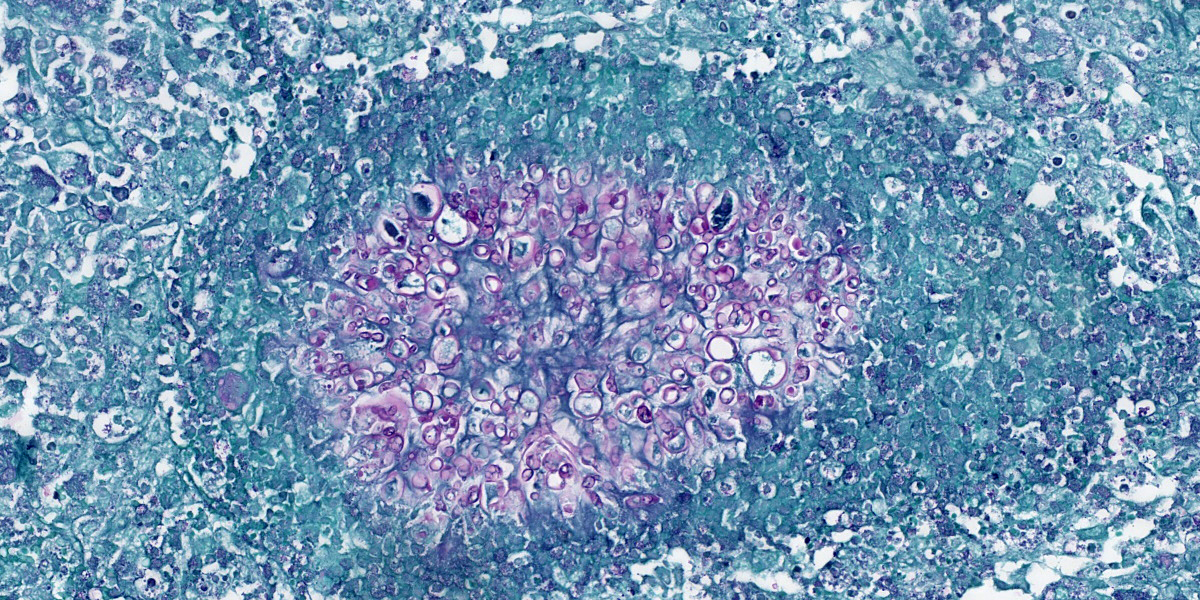
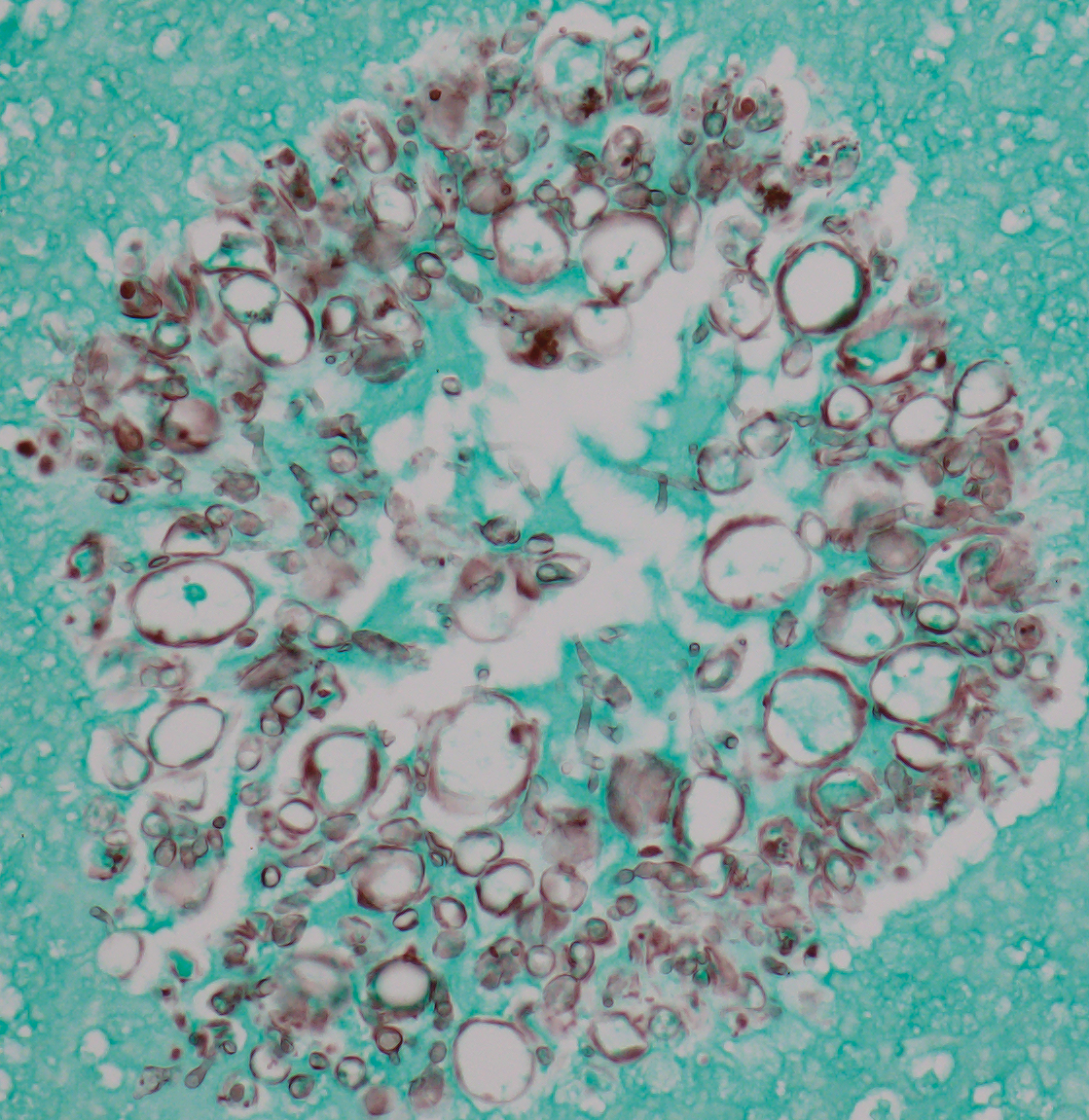
PAS and GMS stains (Figures 1 and 2, respectively) highlight the approximate 2-5 um, polymorphic, fungal hyphae with frequent and bulbous dilatations up to 30 um, consistent with dermatophytic pseudomycetoma.
Contributor’s Morphologic Diagnosis:
Subcutis (mass from the left thorax): Multifocal to coalescing, marked, chronic, pyogranulomas with numerous intralesional fungal hyphae (pseudomycetoma).
Contributor’s Comment:
A pseudomycetoma represents a subcutaneous infection with either bacteria or dermatophytes present in the tissue as granules or grains.7 Dermatophytic pseudomycetoma in horses is a rare form of dermatophytosis with colonization beyond the superficial layers of the skin to the live tissues of the deep dermis and subcutis. The lesions are thought to form following the rupture of an infected hair follicle that results in a granulomatous or pyogranulomatous reaction around the dermatophyte hyphae.8
The most common cause of dermatophytosis in horses is Trichophyton equinum, with less frequent infection by T. mentagrophytes, T. verrucosum, Microsporum equinum, and M. gypseum.10 Dermatophytosis is a common and contagious fungal infection of equine skin affecting horses of all ages, and young animals in crowded environments, and those in hot and humid climates may be over represented.9,10 Infection rarely invades beyond the superficial layers of the skin in healthy animals.9 Although the health status of this horse is unknown, it can be speculated that an immunocompromised state may have predisposed it to the deeper infection and subsequent psudeomycetoma formation. Pseudomycetomas, while rare, are documented in other domestic species, with a predisposition for Persian cats and Yorkshire terriers with Microsporum canis as the most common etiologic agent.8 Given the predominance in Persian cats over other domestic feline species, a genetic deficit in immunity has been a proposed cause.6
With standard hematoxylin and eosin staining, grain or granule-like structures composed of fungal hyphae that are embedded in an amorphous eosinophilic matrix presumed to be antigen-antibody complexes5 are seen to be surrounded by granulomatous or pyogranulomatous inflammation with multinucleate giant cells, and variable lymphoplasmacytic inflammation that are separated by varying degrees of fibrosis. Differential diagnoses include causes of true mycetomas including actinomycetes (actinomycetoma) or fungi (eumyoctic mycetoma).2
Contributing Institution:
University of Illinois at Urbana-Champaign, Veterinary Diagnostic Laboratory
http://vetmed.illinois.edu/vet-resources/veterinary-diagnostic-laboratory/
JPC Diagnosis:
Panniculus and underlying skeletal muscle: Pyogranulomas, multiple with numerous fungal hyphae, Splendore-Hoeppli material, and marked pannicular fibrosis.
JPC Comment:
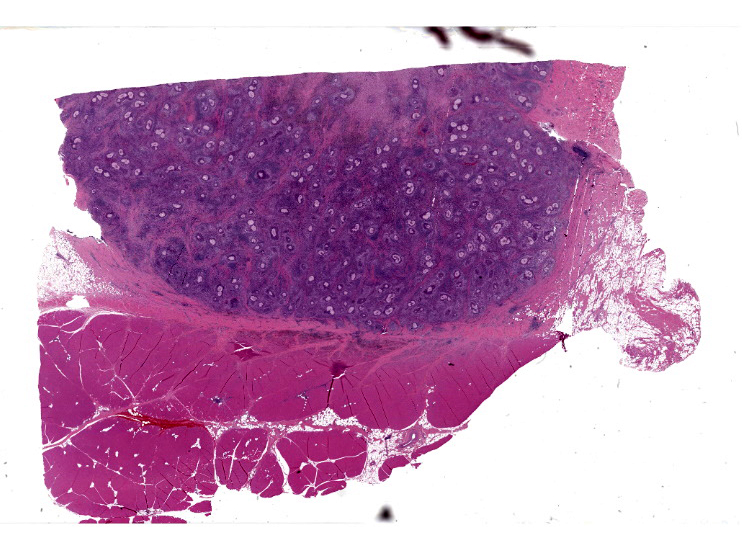
This second case is striking from subgross, with identification of the lesion distribution hardly a diagnostic quandary (figure 2-1). Although special stains were not necessary to arrive at the diagnosis for this case, we found that the methenamine silver (GMS) and periodic acid-Schiff (PAS) stains highlighted fungal elements nicely (figure 2-4, figure 2-5). Significant features include the presence of septate hyphae, chain-like pseudohyphae, and large (12um) pseudogranules.10 Conference participants remarked that the H&E features were convincing for a fungal etiology, but exact speciation was not possible without additional ancillary diagnostics such as PCR or fungal culture. We differed from the contributor therefore in this case by omitting the mycetoma/pseudomycetoma distinction from the morphologic diagnosis. As a final treat for conference participants, Dr. Bruce Williams reminded the group that PAS is pronounced ‘per-eye-OD-ik acid – Schiff’ as the name of the reagent that we use ‘periodically’ for cases has decidedly different pronunciation that is easy to confuse.
As pointed out by the contributor, the location of these fungal pyogranulomas in the deep dermis with extension into the pectoral muscle is unusual for this entity however. Mycetoma should be distinguished from pseudomycetoma by several key features. Mycetomas are fibrotic inflammatory nodules with draining fistulous tracts, and tissue grains of fungal aggregates with fewer hyphal elements surrounded by minimal amounts of Splendore-Hoeppli material and more cement material.5 In contrast, pseudomycetomas are typically multifocal, may lack overt skin changes, are associated with dermatophytes, and typically have more abundant fungal hyphae and Splendore-Hoeppli material present histologically than true mycetomas do.5 The abundant fungal hyphae, multifocal distribution of lesions, and
abundant amorphous eosinophilic material (Splendore-Hoeppli) in this case is most consistent with dermatophytic pseudomycetoma, absent other confirmatory diagnostics. Wider distribution of lesions, to include regional draining lymph nodes, is an occasional finding.1,5
Dermatophytic pseudomycetoma has been rarely reported in the cat1,3,5 and has been previously covered in WSC (see Conference 11, Case 2, 2019-2020 and Conference 11, Case 3, 2008-2009). Persian, and to a lesser extent, Himalayan cats appear to have a predilection that may be explained by a longer hair coat and/or increased susceptibility to dermatophytes secondary to variation in the calprotectin gene which encodes an antimicrobial peptide.1 Dermatophytic pseudomycetoma in shorthair cats has also been described, to include a recent case report from Korea.3 Pseudomycetomas have also been described in the ferret4, though case reports in the horse are sparse in the literature.
References:
- Barrs VR, B?czkowski PM, Talbot JJ, et al. Invasive fungal infections and oomycoses in cats: 1. Diagnostic approach. Journal of Feline Medicine and Surgery. 2024;26(1).
- Cafarchia C, Figueredo L, Otranto D. Fungal diseases of horses. Veterinary Microbiology. 2013;167: 215-234.
- Cho J, Park C, Park J, Yoon JS. Case report: Dermatophytic pseudomycetoma in a domestic Korean short hair cat treated with intralesional injection of amphotericin B and oral terbinafine administration. Front Vet Sci. 2024 Jun 13;11:1402691.
- Giner J, Bailey J, Juan-Salles C, Joiner K, Martinez-Romero EG, Oster S. Dermatophytic pseudomycetomas in two ferrets. Vet Derm 2018: 29:452-e154.
- Gross TL, Ihreke PJ, Walder EJ, Affolter VK. Skin Diseases of the Dog and Cat Clinical and Histopathologic Diagnosis. 2nd ed. Ames, IA: Blackwell Publishing; 2005: 288-291.
- Hargis AM, Ginn P, The integument. Ln: McGavin MD, Zachary JF eds. Pathologic Basis of Veterinary Disease. 6th ed. St. Louis, MO:Mosby Elsevier; 2017: 1079-1144.
- Maudlin EA, Peter-Kenney J. Integumentary. ln: Maxie MG ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. Vol. 1. 6th ed. Philadelphia, PA: Elsevier Saunders. 2016: 649-653.
- Nardoni S Franceschi A & Mancianti F. Identification of Microsporum canis from dermatophytic pseudomycetoma in paraffin-embedded veterinary specimens using a common PCR protocol. Mycoses. 2007;50(3): 215-217.
- Pilsworth R, Knottenbelt D. Common Equine Skin Diseases. Equine Veterinary Journal Ltd, Newmarket, Suffolk, UK; 2006: 52-53.
- Scott, DW, Miller WH. Equine Dermatology. 2nd ed. St. Louis, MO: WB Saunders Co; 2011: 161-163, 171-201.