Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2018-2019
Conference 17
30 January, 2019
CASE IV: 14A310 (JPC 4083744).
Signalment: 13.05 yr, female, Indian rhesus monkey, Macaca mulatta
History: Presented from the field cage in dystocia and an infant was successfully delivered by C-section but the dam died in recovery.
Gross Pathology: Hemorrhagic meninges primarily over the cerebellum, enterocolitis, hemorrhage in both adrenals.
Laboratory results: I-stat Results:
|
Na |
144 meg/l |
ph |
7.152 |
|
K |
3.5 meq/L |
PCO2 |
47.3 mmHg |
|
CL |
111meq/L |
HCO3 |
15.3 g/dL |
|
TCO2 |
18 mmol/L |
BEECF |
12 mmol/L |
|
BUN |
18 mg/dL |
ANGAP20 |
mmol/L |
|
Hct |
45% PCV |
HB |
15.3 g/dL |
Bacterial culture of the meninges: Streptococcus pneumoniae
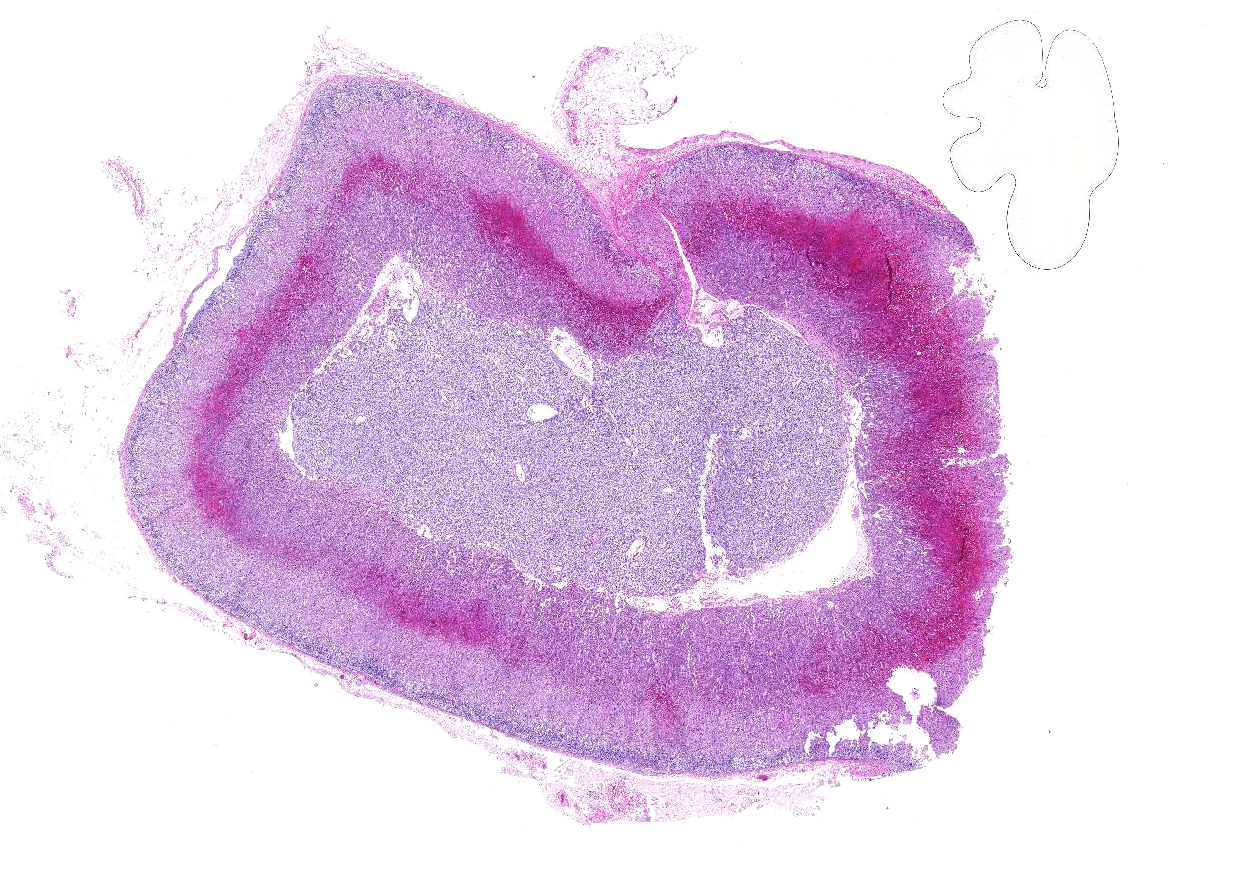
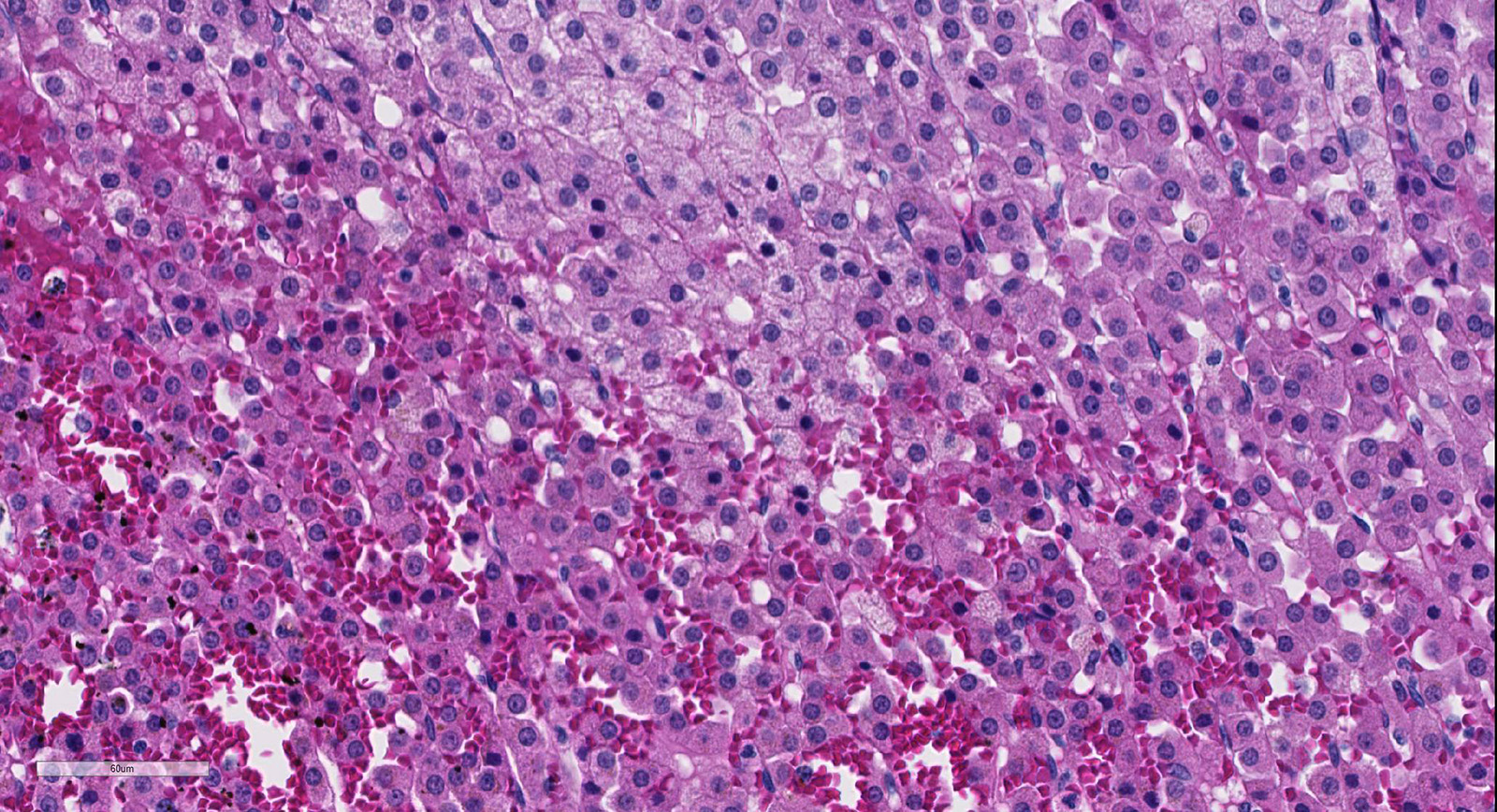
Microscopic Description:
In the cortex of the adrenal, primarily the zona fasiculata is severely congested and hemorrhagic with loss of cortical cell cords and pooling of RBC between surviving the fibrovascular supporting framework. Adjacent cortical cells are swollen and rare capillaries contain minimal aggregates of neutrophils and mononuclear leukocytes.
Contributor’s Morphologic Diagnoses:
Acute severe adrenal cortical hemorrhage with mild degeneration and minimal necrosis, rhesus macaque
Contributor’s Comment: The cesarean section for this animal was complicated by an abscess in the midbrain and meningitis from which Streptococcus pneumoniae was cultured. Meningococcus in humans is often a cause of acute adrenocortical insufficiency2 although we see adrenal hemorrhage infrequently in our primate colony (62 cases in last 30 years). Worldwide, cerebral tuberculosis is the most often associated with pituitary and adrenal dysfunction3. The Waterhouse-Friderichsen syndrome in humans is described as a rare complication of bacteremia due to pneumococci, staphylococci, Neisseria meningitides, Pseudomonas aeruginosa, or Haemophilus influenza and also cytomegalovirus infection that results in systemic hemorrhages including purpura of the skin, with hemorrhage of the adrenal, serous membranes and other organs consistent with development of disseminated intravascular coagulation (DIC).1,4,8 The basis for the hemorrhage, suggested to originate from the venous sinusoids of the medulla and suffuse into the cortex could be due to direct bacterial seeding of the endothelium, DIC, endotoxin-induced vasculitis or hypersensitivity vascultitis.2
Contributing Institution:
Tulane National Primate Research Center
Department of Comparative Pathology
18703 Three Rivers Rd
Covington, LA 70433
http://tulane.edu/tnprc/
JPC Diagnosis: Adrenal gland, zona fasciculata and reticularis: Necrosis, multifocal, marked, with hemorrhage.
JPC Comment: The Waterhouse-Friderichsen syndrome (WFS) is a well-known entity (named for English physician Rupert Waterhouse (1873-1958) and Danish pediatrician Carl Friderichsen (1886-1979) in humans, non-human primates, and several other species. It was first described in 1911 as adrenal hemorrhage and subsequent adrenal crisis related to sepsis.8
In humans, this syndrome is usually associated with fulminant sepsis associated with pneumococcal or meningococcal bacteremia (with Streptococcus pneumoniae and Neisseria meningitidis the most commonly cultured bacilli, respectively) often in patients with splenic disorder or asplenia. Other reported bacterial causes include N. gonorrhoeae, Pseudomonas aeruginosa, E. coli, Hemophilus influenzae, and S. aureus.6 It is often associated with hypotensive shock, disseminated intravascular coagulation, purpura fulminans, and adrenal gland failure. In affected individuals, adrenal hemorrhage may vary from microscopic hemorrhage at the corticomedullary junction to massive, grossly identifiable hemorrhage effacing the entire cortex. Several anatomic factors facilitate the hemorrhage: high rate of blood flow, contribution of several arteries to a single organ-wide capillary plexus, and a single large central vein draining this organ.8 WFS in humans is an emergency situation, clinically characterized by rapidly falling levels of cortisol – high doses of corticosteroids are usually administered as well as antibiotics directed at the bacterial agent.5 Mortality, even in treated cases, often exceeds 50%. While historically a postmortem diagnosis, the adrenal hemorrhage that characterizes WFS in humans may now be identified by ultrasonography and CT scans, increasing the odds of successful treatment.5
In 2009, Hukkanen et al.7 published a retrospective of five cases of systemic inflammatory response syndrome (SIRS) including the Waterhouse-Friedrichsen syndrome, acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC) and multiple organ dysfunction in five cases including both pigtailed macaques and olive baboons. In these animals, predisposing factors were similar to those in humans – major surgery, obstetric complications, and infection. The syndrome is thought to be seen in “high-responders” – subsets of nonhuman primates (and humans) which may produce 10 to 100 fold greater cytokines (IL-1b, IL-6, and IL-8 as well as TnF-alpha in response to infectious stimuli.7
References:
- Adem PV, Montgomery CP, Husain AN, Koogler, TK, Arangelovich V, Humilier M, Boyle-Vavra S, Daum RS. Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children. N Engl J Med 353:1245-2451, 2005.
- Cotran RS, Kumar V, Collins T. (1999). Robins Pathologic Basis of Disease (6th ed) p 1160.
- Dhanwal DK, Kumar S, Vyas A, Saxena A. Hypothalamic pituitary dysfunction in acute nonmycobacterial infections of central nervous system. Indian J Endocrinol Metab 15 (Suppl 3): S233-S237, 2011.
- Emori K, Takeuchi N, Soneda J. A case of Waterhouse-Friderichsen syndrome resulting from an invasive pneumococcal infection in a patient with a hypoplastic spleen. Case Reports in Crit Care 2016; art. ID 4708086.
- Fox B. Disseminated intravascular coagulation and the Waterhouse-Friderichsen syndrome. Arch Dis Childhood 46:680-685, 1971.
- Hale AJ, LaSalvia M, Kirby JE, Kimball A, Baden R. Fatal purpura fulminancs and Waterhouse-Friderichsen syndrome from fulminant Strptococcus pneumoniae sepsis in an asplenic young adult. IDCases 2016: 6:1-4.
- Hukkanen RR, Liggitt HD, Murnane RD, Frevert CW. Systemic inflammatory response syndrome in non-human primates culminating in multiple organ failure, acute lung injury, and disseminated intravascular coagulation. Toxicol Pathol 2009; 37(6):799-904.
- Verzeletti A, Bonfanti C, Leide A, Assalini E, De Francesco MA, Piccineli G, De Ferrari. Streptococcus pneumoniae detection long time after death in a fatal case of Waterhouse-Friderichsen syndrome. Am J Forens Med 2017:38(1)18-19.
- Vincentelli C, Molina EG, Robinson MJ. Fatal pneumococcal Waterhouse-Friderichsen syndrome in a vaccinated adult with congenital asplenia. Amer J Emerg Med 27:751.e3-751.e5, 2009.