Signalment:
Adult, female, Pacific white-sided dolphin (
Lagenorhynchus obliquidens).An approximately 31-year-old, 126 kg, adult female, Pacific white-sided dolphin (
Lagenorhynchus
obliquidens) maintained in a semi-closed, 3.8 million litre captive display pool with a long history of intermittent
gastrointestinal problems was presented with sudden anorexia, abdominal pain, and vomiting. The aging dolphin
had had multiple antibiotic treatments in response to inflammatory blood profiles and inappetence at several public
display institutions and was known as an old dolphin that often goes off. Although gastrointestinal disease had
been suspected, the cause of the recurrent inflammatory changes in the peripheral blood was never definitively
diagnosed. Starting in 2006, budding yeast and pseudohyphae were found on oral and gastric cytology in
association with lethargy, inappetence and recurring inflammatory changes. Antifungal agents including oral
itraconazole and nystatin were used and appeared to speed recovery and decrease the severity of the clinical signs.
Repeated endoscopy of the esophagus and proximal stomach showed no significant lesions, although a thick koilin
coating of the stomach occasionally hampered close examination of the gastric mucosa.
Gross Description:
Necropsy showed an emaciated animal with moderate abdominal distension. On incision of the
abdominal wall, there was approximately 2 L of serosanguineous ascites and an intestinal torsion within the
craniodorsal aspect of the abdominal cavity with displacement of adjoining viscera. Extending from the duodenum
caudally to the midlevel of ileum, there was multifocal to coalescing and occasional segmental yellow discoloration
of the intestinal mucosa with variable amounts of submucosal edema and multifocal caseous to friable yellow white
deposits. In more distal regions of the bowel, the serosa featured a fine cobblestone to granular texture, and was
glistening and stippled to mottled dark red black.
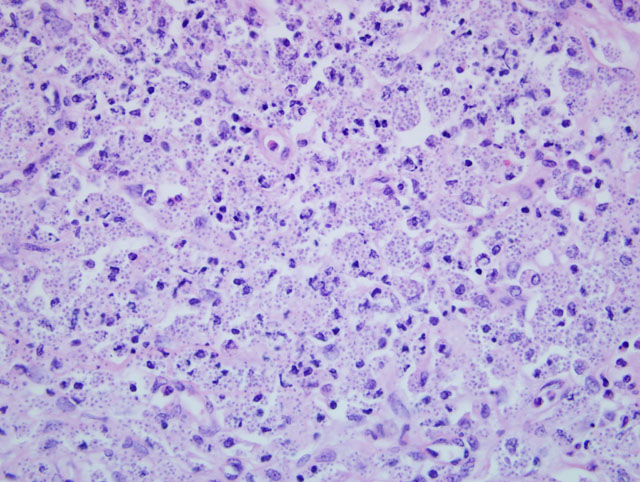
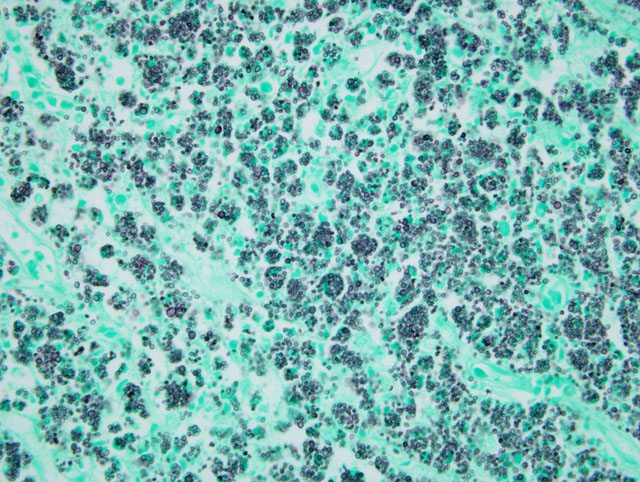
Histopathologic Description:
Jejunum and small intestine: Microscopically, there was marked fibrinosuppurative
and lymphohistiocytic enteritis with florid intralesional yeast.
Morphologic Diagnosis:
1) Jejunum: Torsion, severe, segmental, acute with infarction and
hemorrhage (Gross diagnosis)
2) Small intestine: Enteritis, marked, nodular to diffuse, lymphohistiocytic and fibrinosuppurative, with florid
intrahistiocytic yeast morphologically consistent with
Candida spp.
Lab Results:
Special culture on selective media identified
Candida krusei.
Condition:
Candida krusei
Contributor Comment:
Microscopic assessment of the grossly noted submucosal nodular proliferations in the
multiple segments of small intestine disclosed florid, predominantly intrahistiocytic, yeast morphologically
suggestive of
Histoplasma capsulatum, Blastomyces dermatitidis, Paracoccidioides brasiliensis, Sporothrix
schenckii, Torulopsis (Candida) glabrata, and
Candida spp. In-house culture yielded moderate growth of
Candida
spp. and submission of fresh tissue to a reference lab, the British Columbia Centre for Disease Control, for special
culture on selective media identified
C. krusei, which is considered significant.(1) This organism is the conidal state
of
Issatchenkia orientalilis and is considered a commensal of the mucus membranes and skin of animals and
humans.Â
C. krusei has been occasionally associated with bovine mastitis and there is a single case report of
bronchopneumonia secondary to candidemia in a Holstein heifer. Fatal colonization of a gastrostomy tube has been
reported in a cat.Â
Candida spp. infections in humans are generally localized to the gastrointestinal, urogenital and
respiratory tracts and have been associated with prolonged antibiotic administration, haemodialysis,
chemotherapeutic agents, cancer or other severely debilitating disease, penetrating abdominal trauma, or patients
with indwelling catheters. The pathogenesis of infection is characterized by initial colonization of mucocutaneous
junctions of mucosa of the gastrointestinal tract, then proliferation, and then deeper tissue invasion. Candidiasis has
been documented in a number of marine mammals, including bottlenose dolphins, killer whales, false killer whale,
harbour seals, northern fur seals, California sea lions and a pygmy sperm whale. Infection may present as
disseminated or more localized, such as dermatitis, blowhole erosions, glossitis, pharyngitis, pneumonia, nephritis,
cystitis, or esophagitis.(4) To the best of our knowledge,
C. krusei has not previously been reported in marine
mammals. In this animal, there were no apparent pre-existing conditions within the examined tissues which may
have predisposed or exacerbated infection.
JPC Diagnosis:
1. Intestine: Enteritis, histiocytic, lymphocytic and neutrophilic, multifocally extensive, severe,
with extensive ulceration and myriad intrahistiocytic yeast.
2. Intestine: Enteritis, mesenteritis, and peritonitis, fibrinosuppurative, extensive, severe, with necrosis, hemorrhage
and myriad bacilli.
Conference Comment:
Conference participants favored
Histoplasma capsulatum as the etiology of the fungal
infection. This highlights the potential problems associated with relying on morphology alone in the diagnosis of
many infections. Correlation of histomorphology with culture and other specific techniques can avoid diagnostic
errors. Intrahistiocytic clusters of the yeast-like forms of
Candida can closely resemble Histoplasma in histologic
sections. This is particularly true of
Candida glabrata. Additionally, bacilli, which were demonstrated to be gramnegative,
were present in areas of fibrinosuppurative inflammation and necrosis in the sections examined at
conference.
Participants found this case to be a good opportunity to review the clinicopathologic features of candidiasis. As
noted by the contributor, candidiasis typically presents clinically as a superficial mycosis of mucous membranes
most often in young, debilitated, or immunocompromised animals, or those receiving prolonged courses of antibiotic
therapy. Common anatomic locations of candidiasis include the mouth, esophagus, crop, and proventriculus in
birds; the oral mucosa in mammals; and the stomach in piglets.(2) Birds are affected by
Candida species more
frequently than mammals. Grossly, infection by
Candida results in a white pseudomembrane overlying mucous
membranes. Histologically, pseudohyphae, blastoconidia, hyphae, and yeast-like organisms are present, and there is
often necrosis or ulceration.
Conference participants also discussed specifics of virulence and immunity in candidiasis.Â
Candida species have the
ability to change phenotypes in a random and reversible manner in response to changes in the host environment
resulting from antibiotic treatment, immune response, or altered host physiology. The phenotypic variants can
exhibit changes in colony morphology, cell shape, antigenicity, and virulence. Virulence is related to the organisms
ability to adhere to cells, and adherence to host cell is mediated by several classes of adhesins. One class of
adhesions is an integrin-like protein which binds to arginine-glycine-aspartic acid groups on fibrinogen, fibronectin,
and laminin. A second adhesion class, resembling transglutaminase substrates, binds to epithelial cells; and a third
group of agglutinins bind to endothelial cells or fibronectin. Several secreted enzymes, such as aspartyl proteinases,
aid in tissue degradation, facilitating organism invasion.Â
Candida species also secrete adenosine to block neutrophil
degranulation, thus preventing the production of free oxygen radicals which would be damaging to the organisms.(2)
Both innate and cell-mediated immunity are necessary for clearing infections. Neutrophil and macrophage
phagocytosis and subsequent oxidative destruction of the yeast are important in preventing establishment of
infection. The filamentous form of this organism escapes the phagolysosome and replicates in the cytoplasm of
infected cells.Â
Candida yeasts stimulate dendritic cell production of IL-12 to a greater degree than the filamentous
form, resulting in a protective T
H1; in contrast, the filamentous form induces a non-protective T
H2 response.(3) Similar
to other fungi, this organism elicits a T
H17 response, resulting in recruitment of neutrophils and monocytes to the
site of infection. For a thorough review of the general pathology involved in the various T-cell responses, readers
are encouraged to review
WSC 2008-2009, Conference 16, Case 4.
References:
1. Hager JL, Mur MR, Hsu S.Â
Candida krusei fungemia in an immunocompromised patient.Â
Dematol Online J.
2010;16(4):5.
2. McAdam AJ, Sharpe AH. Infectious diseases. In: Kumar V, Abbas AK, Fausto N, Aster JC, eds.Â
Robbins and
Cotran Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Elsevier Saunders; 2009:382-384.
3. Reidarson, T, McBain, J, Dalton, L, Rinaldi, M. Mycotic Diseases. In: Dierauf LA, Gulland FMD, eds. CRC
Handbook of Marine Mammal Medicine. 2nd ed. Washington D.C.: CRC Press; 2001:337-352.