Wednesday Slide Conference, 2025-2026, Conference 3, Case 3
Signalment:
5-year-old, male castrated, Rottweiler, canine.History:
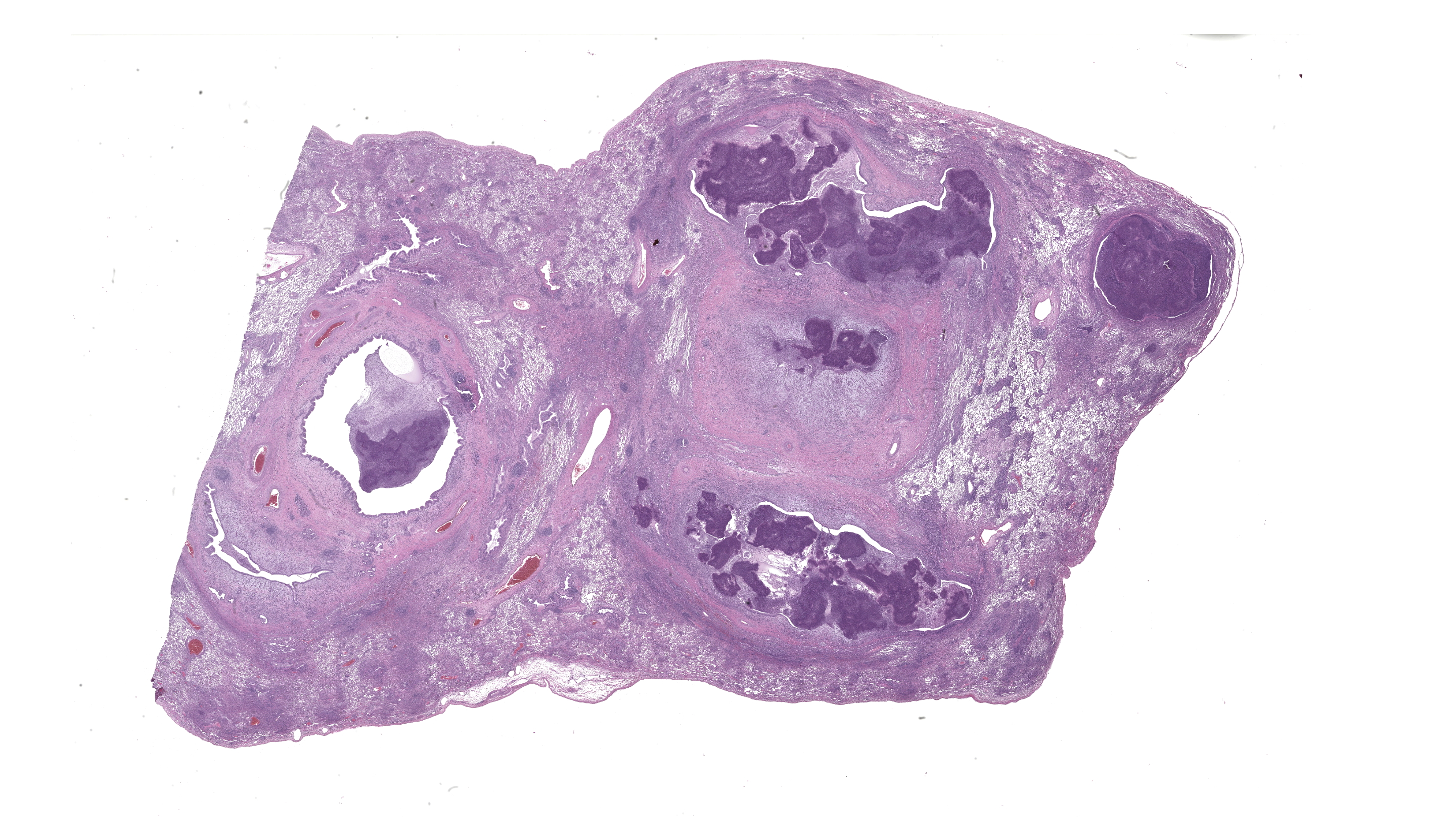
The dog was presented to the Auburn University Bailey small animal teaching hospital with one week history of a wet productive cough. Thoracic radiographs showed pneumonia and CBC revealed eosinophilia. On thoracic CT, there was severe bronchiectasis within the accessory lung lobe and mild focal bronchiectasis within the left caudal lung lobe. Bacterial and fungal culture were negative on bronchoalveolar lavage fluid. The patient was sent home on marbofloxacin and prednisone. The owners have noted the cough has approved with treatment but still not ideal. Three months later, the dog returned to the teaching hospital and the right caudal, right accessory, and left caudal lung lobes were removed and submitted for histopathological examination.Gross Pathology:
Right caudal, right accessory, and left caudal lung lobes had multiple, markedly dilated bronchi or bronchioles filled with light pink to brown inspissated material. The walls of several bronchi was markedly thickened and the intervening lung parenchyma was multifocally collapsed.Laboratory Results:
Bronchoalveolar lavage fluid submitted for bacterial and fungal cultures was negative.Microscopic Description:
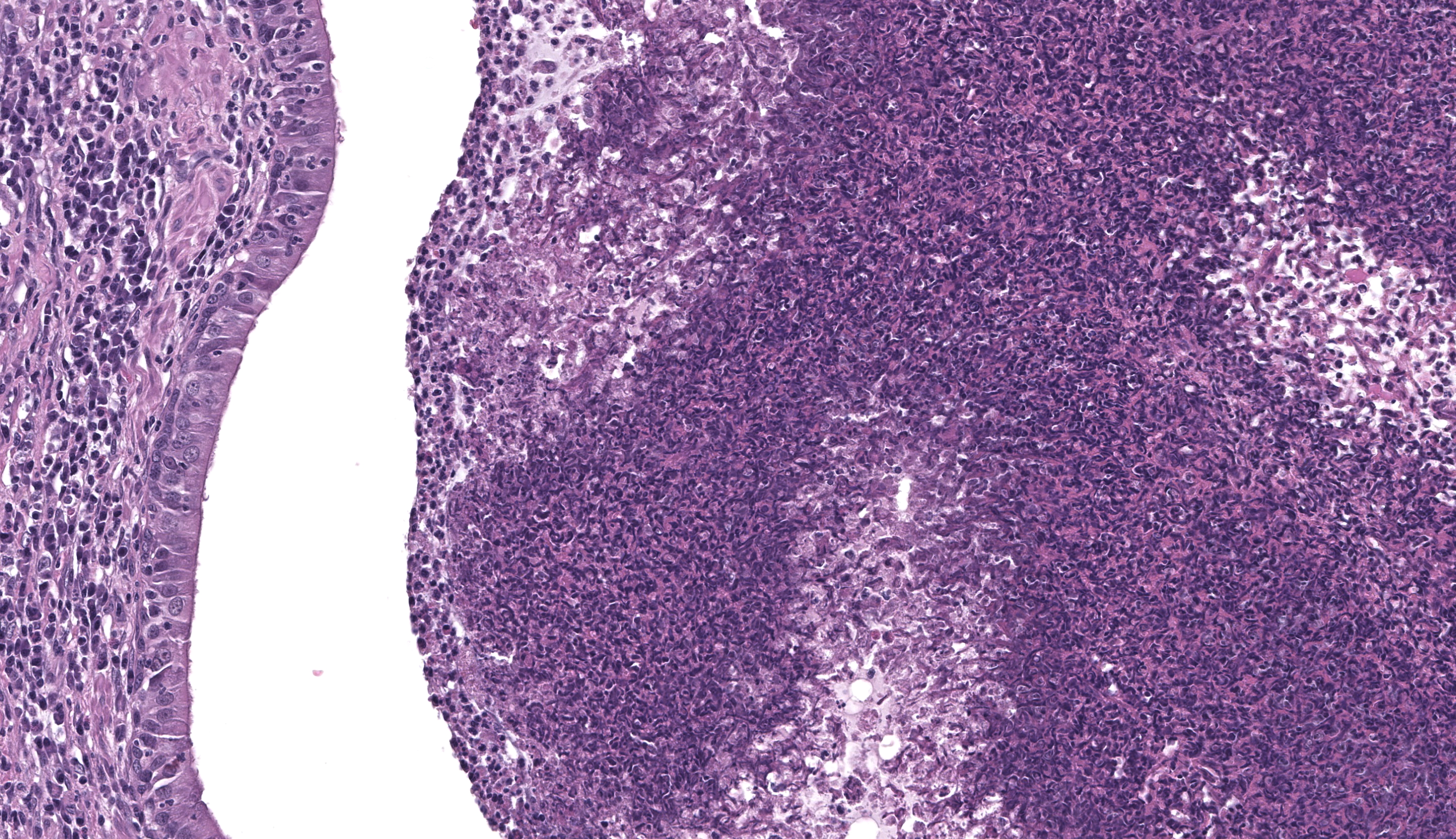
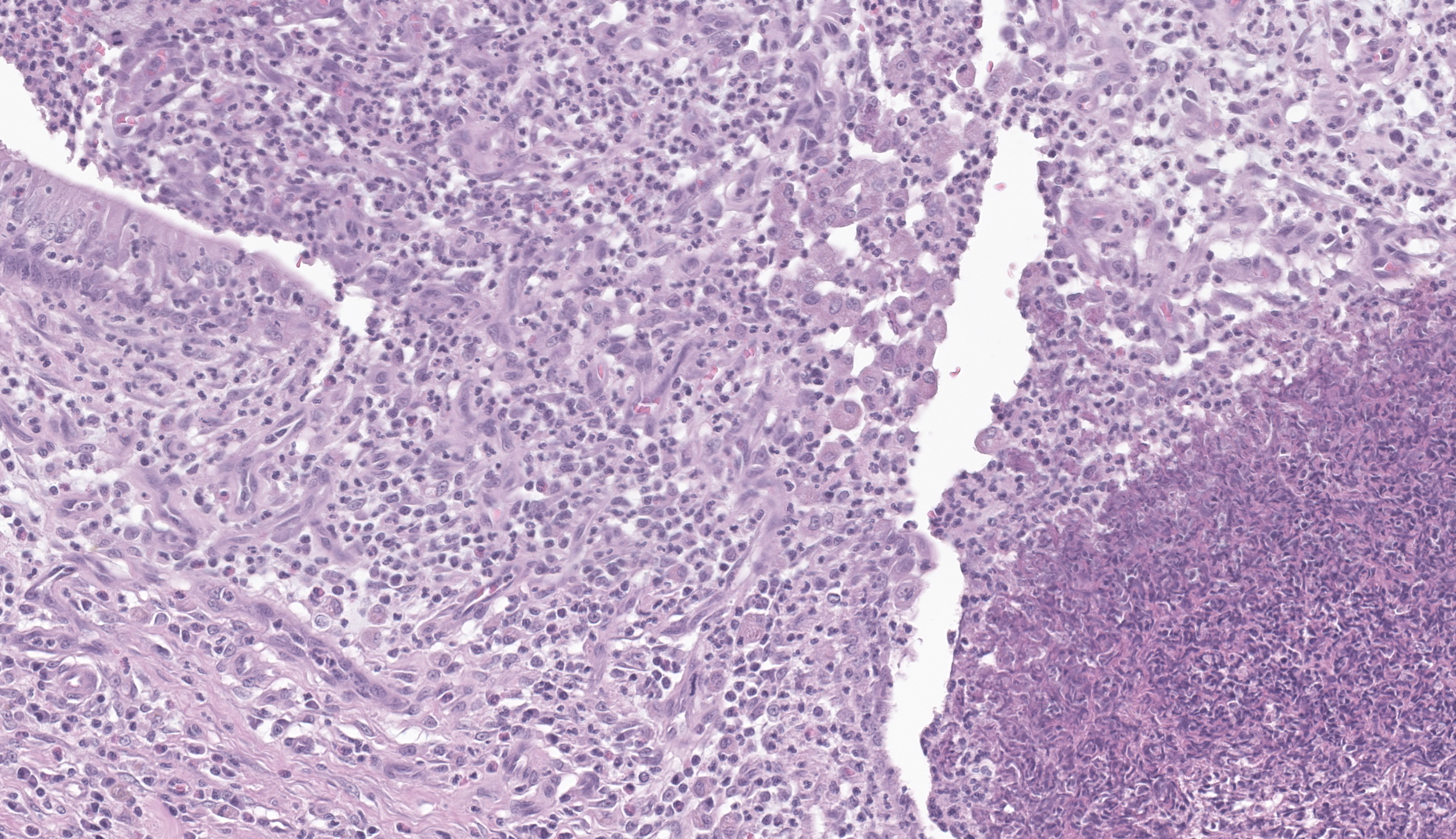
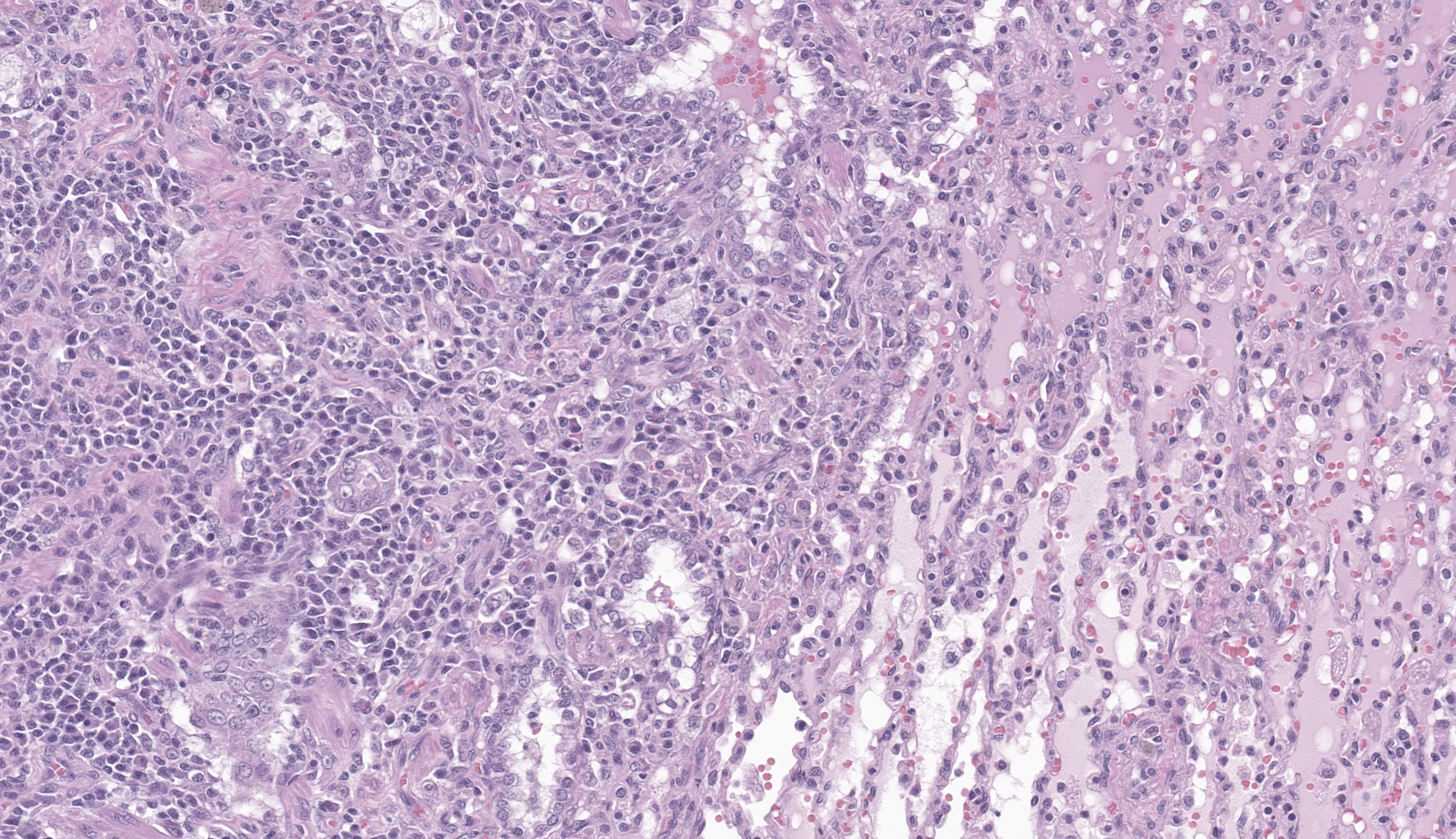
Diffusely, bronchioles and bronchi are markedly ectatic and filled with large amount of inspissated material composed of larger numbers of eosinophils, degenerate neutrophils, admixed with macrophages, mucin, serum, sloughed epithelial cells and eosinophilic cellular and basophilic nuclear debris. Large numbers of similar inflammatory cells also infiltrate the bronchial wall. The lining mucosal epithelium is diffusely moderately hyperplastic or occasionally eroded or ulcerated. Multifocally, bronchi and bronchioles are also surrounded by moderate numbers of eosinophils, neutrophils and macrophages. There is moderate hyperplasia of bronchus-associated lymphoid tissue. Inflammatory exudate multifocally extends into the adjacent alveolar lumina. The adjacent normal alveoli contain moderate numbers of neutrophils, eosinophils and intraalveolar macrophages. The lung parenchyma surrounding the markedly expanded bronchi is multifocally collapsed with closely apposed alveolar septa. Multifocally, there is mild pleural fibrosis. Occasionally, there is mild smooth muscle hypertrophy of bronchioles and tunica media of small caliber blood vessels. Bacterial and fungal organisms are not observed by Gram and GMS stains, respectively.Contributor's Morphologic Diagnoses:
Lung; right caudal lung lobe, right accessory and left caudal lung lobes: Severe, chronic, multifocal bronchiectasis and bronchiolectasis with marked eosinophilic, suppurative bronchitis and bronchiolitis.Contributor's Comment:
Eosinophilic bronchopneumopathy (EBP) is an uncommon, chronic, usually steroid-responsive condition of young adult dogs. EBP has been described in several breeds of dogs with Siberian huskies and Alaskan malamutes being overrepresented.5 The presentation varies from mild to severe, intermittent to chronic, and self-limiting to sometimes fatal. The most common clinical sign is persistent cough, followed by gagging and retching. Other common clinical symptoms include dyspnea, exercise intolerance and nasal discharge that is usually yellow-green to mucopurulent. Radiographic findings include diffuse bronchointerstitial pattern, peribronchial cuffing with or without bronchiectasis.5 Approximately 50% of the dogs have peripheral eosinophilia2. The disease is characterized by eosinophilic infiltration of the lung and bronchial mucosa with epithelial hyperplasia, ulceration or squamous metaplasia. The destruction of the walls of the airways leading to bronchiectasis has also been reported.5The cause of EBP is unknown, however it is thought to be due to hypersensitization to aeroallergens. Immunological and immunohistochemical studies show that bronchoalveolar (BAL) fluid contains decreased numbers of CD8+ T cells, while CD4+ T cell number is increased in the bronchial mucosa and pulmonary interstitium. The predominance of CD4+ T cells supports the role of a dominant Th2 immune response in the affected dogs.4 The dog in the current case was presented with characteristic clinical signs and blood eosinophilia. Based on the imaging findings of bronchiectasis with negative bacterial and fungal culture, EBP was the primary differential. In most cases, the cytological evaluation of BAL fluid usually reveals marked eosinophilia, which along with imaging findings is sufficient to confirm the diagnosis of EBP. The macroscopic lesions vary from no discharge to the presence of abundant yellow-green mucopurulent material within bronchi or bronchioles, thickening of bronchial and bronchiolar walls, bronchiectasis and consolidation of adjacent parenchyma. Typical histologic findings include eosinophilic infiltrate beneath or within the mucosal epithelium and varying degrees of mucosal thickening, infiltration by other inflammatory cell types, collagenolysis, and fibrosis. In cases of extensive involvement of lung parenchyma, there is diffuse eosinophilic and granulomatous infiltrate, with focal eosinophilic granulomas centered on necrotic tissues can be present.3 The diagnosis of EBP was confirmed only after ruling out other causes of eosinophilic infiltrate in the lung and negative bacterial and fungal culture. The tracheobronchial parasites Crenosoma vulpis, Eucoleus aerophilus, Oslerus osleri; the lungworm Angiostrongylus vasorum and Filaroides hirthi; occult Dirofillaria immitis infection are the main differential diagnosis.2 There was no evidence of parasite eggs, larvae or adults in the examined sections. The lesions were primarily centered on bronchioles and bronchi, with mild to moderate involvement of the pulmonary parenchyma. A rare condition called eosinophilic pulmonary granulomatosis is also characterized by similar clinical signs including blood eosinophilia should be included in the differential diagnoses list, but in this condition, there are nodular necrotizing lesions formed by eosinophils, epithelioid macrophages, type II pneumocyte proliferation, which were absent in this case.3 Other causes of eosinophilic infiltrate in the lung parenchyma include lymphomatoid granulomatosis, carcinomas and lymphomas. The mainstay of treatment for EBP is the long?term administration of corticosteroids such as prednisolone.1 In summary, the clinical diagnosis relies on a typical history of chronic respiratory distress, demonstration of bronchopulmonary eosinophilia by cytology or histopathologic examination, and exclusion of known causes of lower airway eosinophilia.
Contributing Institution:
Auburn University http://www.vetmed.auburn.edu/academic-departments/dept-of-pathobiology/JPC Diagnoses:
Lung: Bronchiolitis, eosinophilic and granulomatous, chronic, multifocal to coalescing, severe, with bronchiolectasis, necrotizing alveolitis, and Type II pneumocyte hyperplasia.JPC Comment:
Today’s third case took conference participants on another “Magic School Bus”-esque trip into the lungs in the form of a disease that has more names than it knows what to do with: Eosinophilic Bronchopneumonopathy. Conference discussion started off with a brief nod to the Rottweiler breed and its storied history as descendants from Roman dogs that moved with their humans across the Alps and ultimately into Rottweil, Germany. The dogs ultimately became known as “Rottweiler metzgerhunds”, and were common companions of butchers, where these stocky canines would be seen pulling carts of meat for sale through the streets of Rottweil. Despite this case of eosinophilic bronchopneumonopathy being in a Rottweiler, however, they are not considered a predisposed breed. Alaskan Malamutes and Siberian Huskies, however, are.This case provided a fantastic example of true bronchiectasis with abundant inflammation and debris filling the larger airways in section. Eosinophilic bronchopneumopathy is one of the most common diseases associated with bronchiectasis in dogs, with over a quarter There was some discussion about the brightly eosinophilic material admixed with the eosinophils filling these airways, which was interpreted as likely to be a combination of necrotic eosinophils and major basic protein. A more substantial review of eosinophils was covered in last week’s conference (Conf 2, Case 3), so that topic won’t be belabored further today.
This condition is considered to be both “eosinophilic” and “granulomatous” due to the profound presence of both eosinophils and macrophages. In the course of this disease, there is an upregulated Th2 response, favoring CD4+ T-helper cells over those that are CD8+. The Th2 response is important for fighting extracellular parasites and allergens via production of cytokines like IL-4, IL-5 (chemotactic for eosinophils), and IL-13.6 These cytokines trigger IgE antibody production, recruit and activate cells such as eosinophils and mast cells, increase mucus production, and promote tissue healing. While protective against parasites and involved in wound healing, an overactive Th2 response can cause chronic inflammatory conditions.6 Despite being a common condition in dogs, the exact cause of eosinophilic bronchopneumonopathy in dogs is not known. There are conflicting papers that argue for or against an association with heartworm disease, although there isn’t much argument that heartworm disease is not the only cause of this condition, and it is ultimately suspected that EBP is due to a hypersensitivity reaction of some kind.3,4,5
References:
- Canonne AM, Bolen G, Peeters D, Billen F, Clercx C. Long?term follow?up in dogs with idiopathic eosinophilic bronchopneumopathy treated with inhaled steroid therapy. J Small Anim Pract. 2016; 57(10):537-542.
- Caswell JF, Williams KJ. Respiratory system. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. Vol 2. 6th ed. Philadelphia, PA: Elsevier Saunders; 2016: 465-590.
- Clercx C, Peeters D. Canine eosinophilic bronchopneumopathy. Vet Clin North Am Small Anim Pract. 2007;37(5):917-935.
- Clercx C, Peeters D, German AJ, Khelil Y, McEntee K, Vanderplasschen A, Schynts F, Hansen P, Detilleux J, Day MJ. An immunologic investigation of canine eosinophilic bronchopneumopathy. J Vet Intern Med. 2002;16(3):229-237.
- Clercx C, Peeters D, Snaps F, Hansen P, McEntee K, Detilleux J, Henroteaux M, Day M. Eosinophilic bronchopneumopathy in dogs. J Vet Intern Med. 2000; 14(3):282-291.
- Kokubo K, Onodera A, Kiuchi M, Tsuji K, Hirahara K, Nakayama T. Conventional and pathogenic Th2 cells in inflammation, tissue repair, and fibrosis. Front Immunol. 2022;13:945063.