Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2018-2019
Conference 11
5 December, 2018
CASE II: Case #1 (JPC 4085967)
Signalment: 16-month-old, female, European shorthair cat
History: The cat showed a non-healing wound at the right forelimb over a few weeks. A treatment with NSAID´s and antibiotics didn’t show any improvement. Therefore a biopsy was taken for microscopic investigation.
Gross Pathology: The specimens showed a moderate alopecia and some crusts.
Laboratory results: Molecular biological examination:
- PCR for Cowpox virus: positive
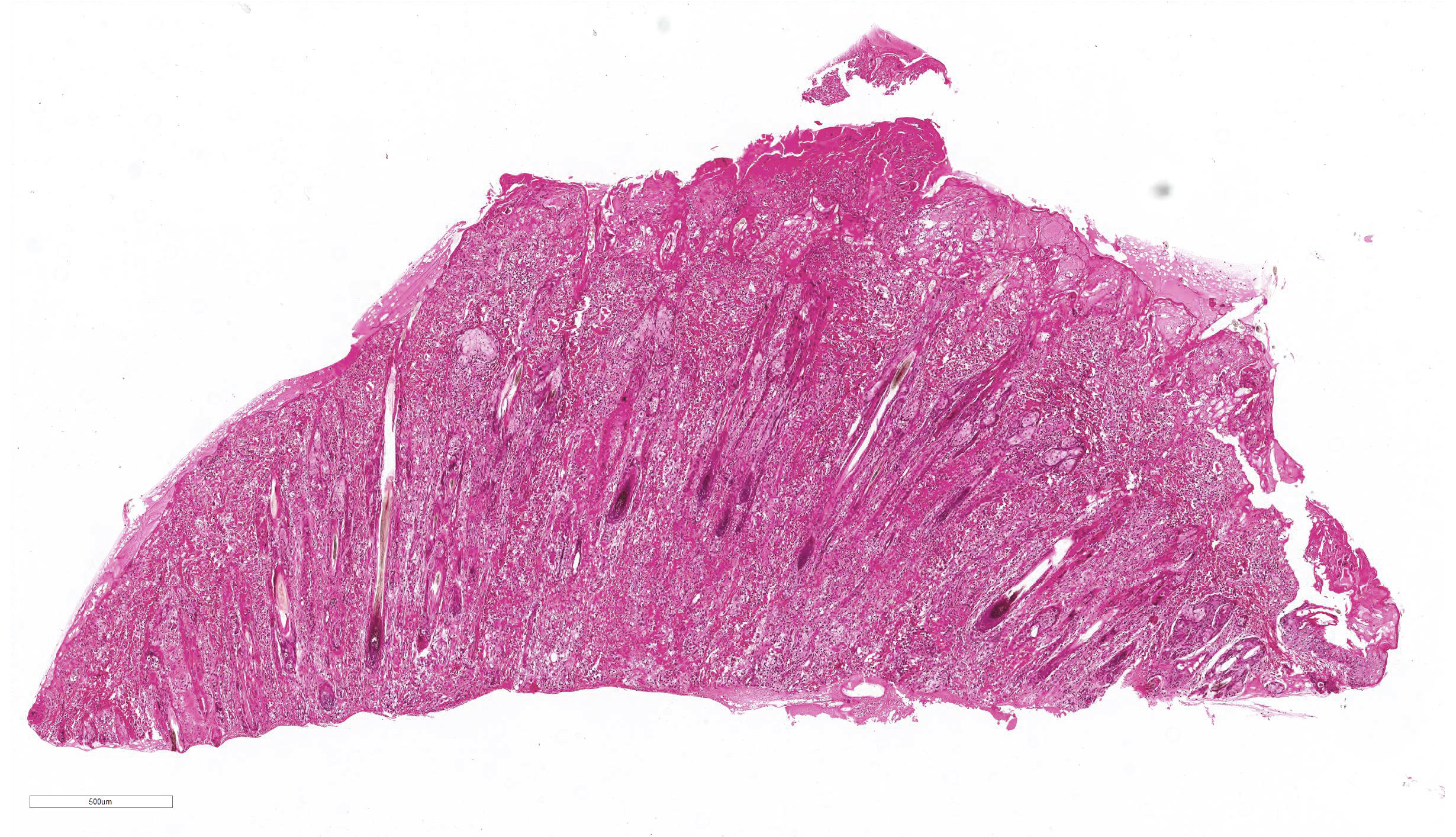
Microscopic Description:
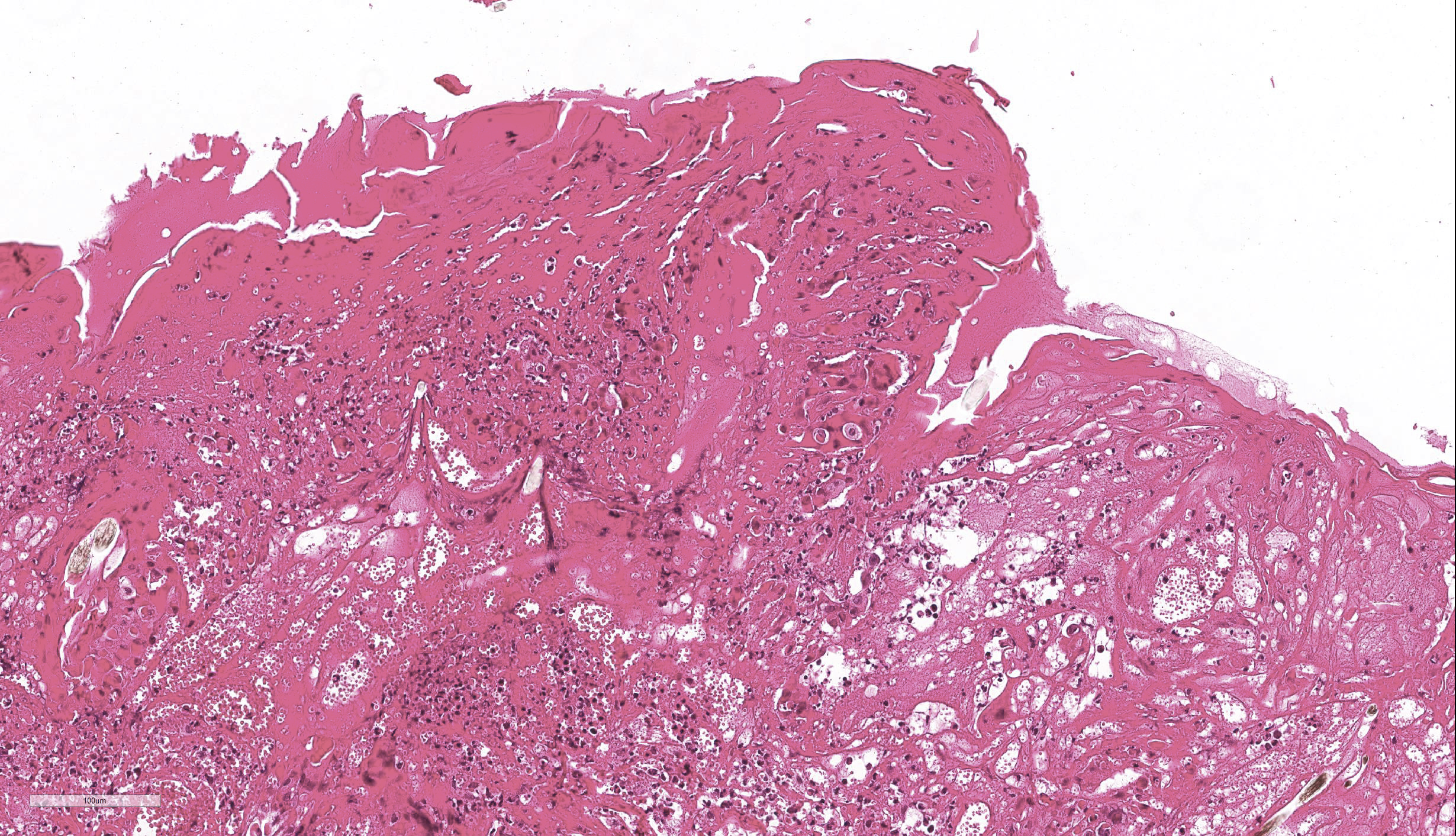
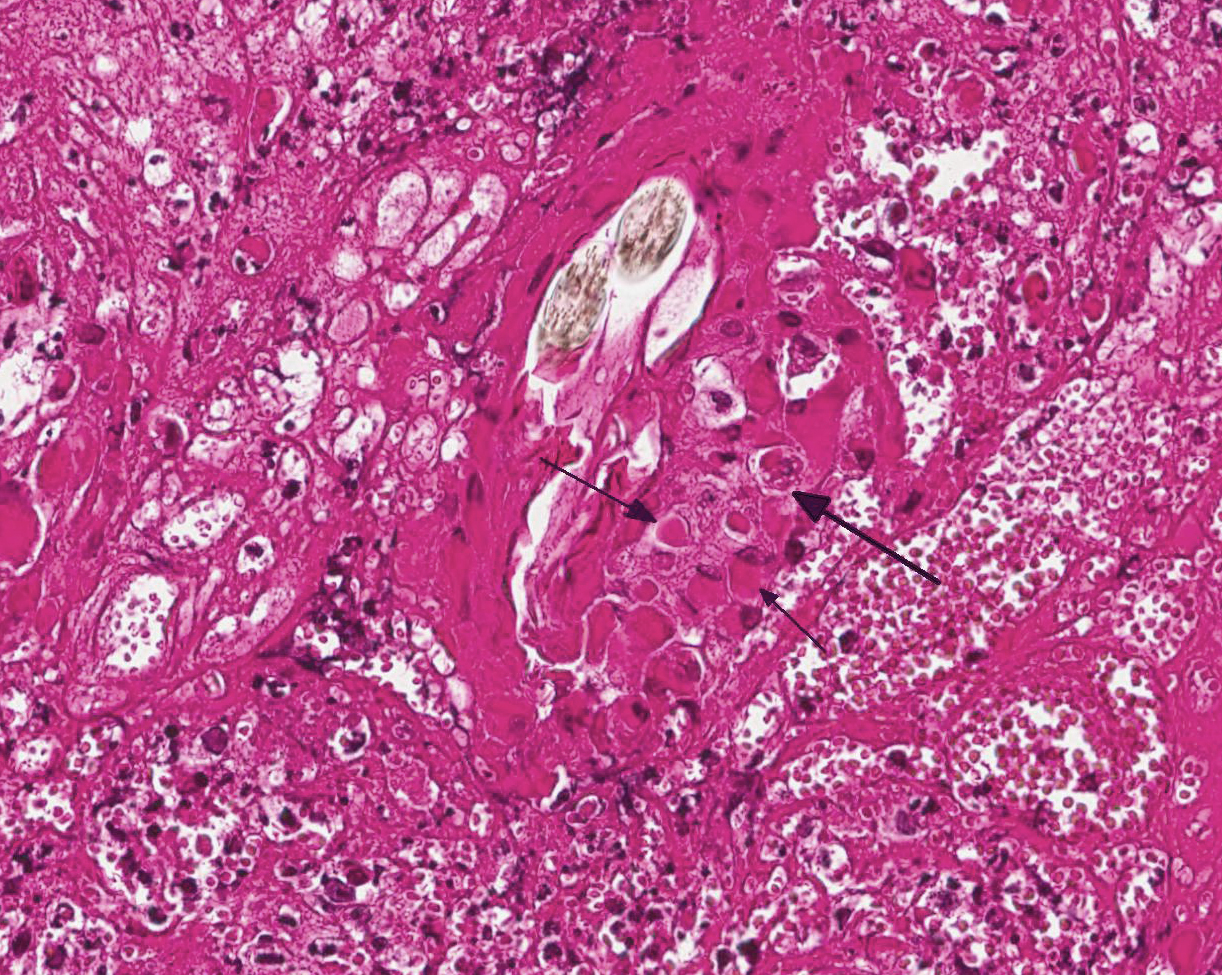
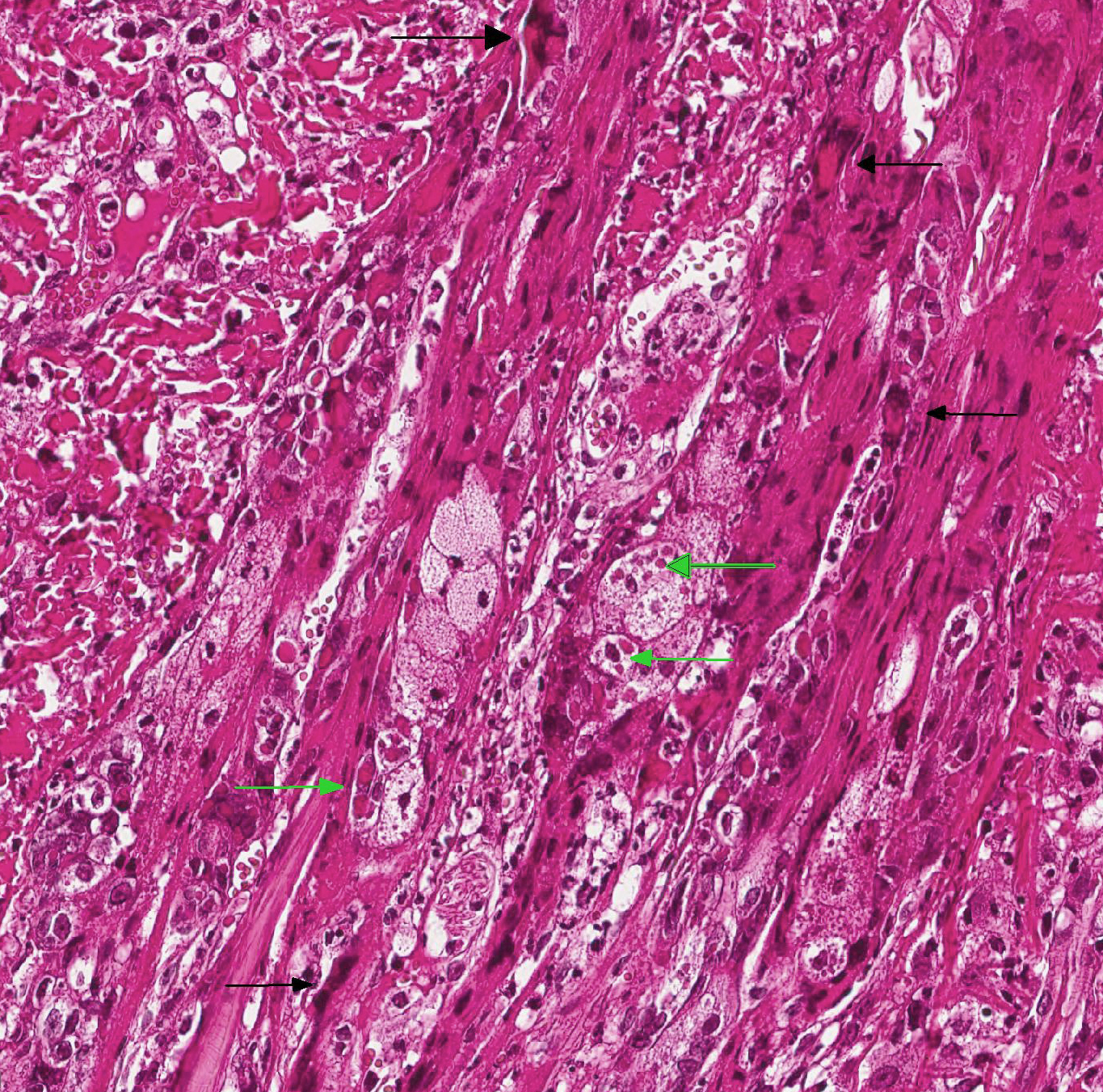
- Epidermis: diffusely covered by plasmatic components; nearly diffuse severe erosions and ulcerations multifocal with serocellular crusts containing a high mount of neutrophils; multifocal moderate intracellular edema up to ballooning degeneration and necrosis of the keratinocytes; multifocal eosinophilic intracytoplasmic inclusion bodies within the keratinocytes
- Dermis: severe infiltration with marked numbers of neutrophils, some lymphocytes, plasma cells and macrophages; multifocal severe necrosis with degenerate neutrophils and cellular and karyorrhectic debris; multifocal moderate hemorrhages
- Adnexa: disseminated severe perifollicular infiltration with marked numbers of neutrophils, some lymphocytes, plasma cells and macrophages, multifocal with complete destruction of the adnexa; multifocal eosinophilic intracytoplasmic inclusion bodies within the keratinocytes of the hair follicle
Contributor’s Morphologic Diagnoses:
Haired skin: Dermatitis, purulent and necrotizing, erosive and ulcerative, severe, with eosinophilic intracytoplasmic inclusion bodies within keratinocytes
Contributor’s Comment: Etiology: The cowpox virus is a member of the genus Orthopoxvirus in the family Poxviridae. The reservoir hosts are rodents from which the virus spreads to other animals, for example cows, cats (including large felids), zoo animals (rhinoceroses, elephants, okapis) and humans.9 In cats, it usually causes a regional viral dermatitis and is often a more severe disease than in cattle or humans. There is an increased incidence in the autumn, which may reflect the increased size and activity of wild rodents in this time of the year.1
The primary lesion after cutaneous infection is usually an ulcerating, erythematous, crusted macule or plaque on the head, neck, or forelegs that occurs after 3-6 days.9 After a viremia, pyrexia, anorexia and depression widespread secondary lesions develop within 10 days to a few weeks.1,5 Like the primary lesion, these first appear as small erythematous macules, ultimately forming ulcerated papules. Sometimes, vesicles are found on the tongue, the mouth or inner aspect of the pinna. Approximately 20 per cent of affected cats show a mild infection of the upper respiratory tract. After three weeks the cutaneous scabs dry and fall off.2 Typical microscopic findings are ulceration, serocellular crusts, ballooning degeneration of keratinocytes in epidermis and hair follicles with large intracytoplasmic eosinophilic inclusions and a secondary necrosis and infiltration with inflammatory cells.6
There are reports about some cases with more severe clinical signs, especially with a severe necrotizing or interstitial pneumonia, necrotizing rhinitis and/or generalized skin lesions. These are either described as atypical infections or are associated with secondary bacterial infection or an underlying immunosuppression like FIV, parvovirus and FeLV infections, debilitative disease or treatment with corticosteroids.8,12,13,14 Macroscopic differential diagnoses for this condition are facial and nasal dermatitis and stomatitis associated to feline herpesvirus 1, cutaneous lymphoma, autoimmune dermatoses, such as pemphigus foliaceus, cutaneous bacterial, fungal or parasitic infections and physicochemical injuries.7,8 Because of the intracytoplasmic inclusion bodies, there are no histological differential diagnoses.
Furthermore, cowpox virus infection is zoonotic and there exist several reports of the virus being transmitted from cats to human beings.8,14,15Lesions are similar to those in cats and are usually associated with a cat scratch.8,14
Contributing Institution:
Institut für Veterinär-Pathologie, Veterinärmedizinische Fakultät Leipzig, Universität Leipzig,
Germany (http://www.vetmed.uni-leipzig.de/ik/wpathologie)
JPC Diagnosis: Haired skin: Dermatitis, necrotizing, diffuse, severe with epithelial ballooning degeneration,and numerous intracytoplasmic viral inclusions.
JPC Comment: Few medical or veterinary students have not heard the story of Edward Jenner, the milkmaids, and his discovery of the correlation between inoculation with cowpox and resistance to smallpox. In a time in which myths fall quickly and hard, the long-held attribution of one of the early vaccine discoveries has been recently called into question. A 2018 article in the New England Journal of Medicine3 ascribes the important observation to the physician towhom Jenner was actually apprenticed, Dr. John Fuster, who two years earlier in 1768, began inoculating people against smallpox.” It was a conversation with a farmer that Fuster inoculated ineffectually that led to the connection between smallpox and cowpox, when the farmer exclaimed, “I have had the Cow Pox lately to a violent degree, if that’s any odds.” Jenner confided about the finding to a friend later that year, but would not travel to London to gain fame as the inventor of the vaccine until 1770.
Even the identity of the virus used by Jenner et al. has been called into question. While the story of the “unrivaled” (i.e., unpocked) complexions of the milkmaids in the area at that time is legend, even the use of the cowpox virus in early vaccinations has been called in to question. The widespread exchange and mixing of vaccines and “lymph” in the US in the early 1900s resulted in vaccines today that likely would contain viral determinants of many vaccines in use around the world at that time. Interestingly, no trace of cowpox has been identified in vaccines tested from that time or today’s derivatives. The active virus appears to be the vaccinia virus, closely related to cowpox, but instead isolated from horses.5
Today, cowpox viruses are distributed throughout Asia and Europe, except for Ireland. Wild rodents, predominantly voles, are the reservoir of these viruses; hunting cats are accidentally infected by their prey.9 Historically, cattle (likely infected by rodent contact) have been the primary source for zoonotic infections; however, within the last decade, cats have been primarily described as the source of human infections. Wild rodents are the primary source for the cat; pet rats have been rarely been incriminated in human infections.9
While generally considered to be a cutaneous infection, fatal generalized systemic infections with cowpox virus have been seen in immunosuppressed cats, as well as a single human case report following immunosuppressive corticosteroid therapy. The effects of concurrent immunosuppressive viruses such as file T virus, retrovirus, parvovirus may also exerts adverse effects by promulgated concurrent bacterial infections.9
A number of atypical cases of cowpox in cats have been identified in the literature. Necrotizing and proliferative pneumonia has been seen in the absence of cutaneous lesions in domestic cats and wild felids. A series of cases in cats in which the cutaneous lesions were present on the hindlimbs or tail was reported by Jungwirth et al.10 In a Denmark zoo which has reported seasonal recurrence of cowpox virus outbreaks in captive cheetahs, two of nine (22%) died of generalized disease or pulmonary infection.17
Finally, a fatal outbreak of a novel orthopoxvirus was reported in 2017, in which phylogenetic analysis revealed the virus to be distantly related to cowpox, and more closely related to ectromelia virus.4 Autopsied macaques demonstrated interstitial pneumonia with necrosis of bronchial epithelium; lymphoid necrosis of the spleen and lymph node, and numerous ulcers in the skin and upper GI tract. Rodents in the facility demonstrated serologic (IGG) to the putative poxvirus, but the virus was not isolated from trapped rodents. A subsequent report of cutaneous infection by a virus within the same cluster as this putative novel orthomyxovirus was subsequently reported.11
The attendees noted the presence of numerous multinucleated epithelial cells, which are not commonly seen in poxviral infections; their significance or etiology in this case is not apparent. The large areas of profound necrosis of the epidermis led some attendees to question whether vascular lesions, such as may be seen in other orthopoxviral infections, such as ectromelia, might have been present.
References:
- Bennett M, Gaskell CJ, Gaskell R M, Baxby D, Gruffydd-Jones TJ. Poxvirus infection in the domestic cat; some clinical and epidemiological observations. Vet Rec. 1986;118:387–390
- Bennett M, Gaskell CJ, Baxbyt D et al. Feline cowpox virus infection. J Small Anim Pract 1990; 31:167–73.
- Boylston, AW. The myth of the milkmaid. NEJM 2018; 378(5):414-415.
- Cardeti G, Gruber CEM, Eleni C, Carietti F, Castiletti C, Manna G, Rsosone F, Giombini E, Seileri M, Lapa D, Puro V, Di Caro A, Lorenzetti R, Scicluna MT, Grifoni G, Rizzoli A, Tagliapietra V, De Marco L, CApobianchi MR, Autorinao GL. Fatal outbreak in Tonkean macaques caused by possibly novel orthopoxvirus, Italy, January 2015. Emerg Inf Dis 2017; 23(12)1941-1949.
- Damaso CR. Revisiting Jenner’s mysteries, the role of the Baugency lympho in the evolutionalry path of ancient smallox vaccine. Hist Rev 2018; 18(2): 55-63. For the
- Gaskell RM, Gaskell CJ, Evans RJ, Dennis PE, Bennett AM, Udall ND, Voyle C, Hill TJ. Natural and experimental poxvirus infection in the domestic cat. Vet Rec. 1983;112:164–170.
- Gross TL, Ihrke P, Walder E, Affolter VK. Ulcerative and crusting diseases oft the epidermis. In: Skin diseases of the dog and cat: clinical and histopathologic diagnosis. 2nd ed. Blackwell Science. 2005; 116-135.
- Hargis AM, Ginn PE. Feline herpesvirus 1-associated facial and nasal dermatitis and stomatitis in domestic cats. Veterinary Clinics of North America: Small Animal Practice Vet Clin N Am-Small 1999; 29:1281–90.
- Herder V, Wohlsein P, Grunwald D et al. Poxvirus infection in a cat with presumptive human transmission. Vet Dermatol 2011; 22:220–4.
- Jungwirth N, Puff C, Koster K, Mischke R, Meyer, H, Stark, A, Thoma, B, Zoller G, Seehusen F, Hewicker-Trautwein M, Beineke A, Baumgartner W, Wohlsein P. Atypical Cowpox virus infection in a series of cats. J Comp Path; 2018 158:71-76
- Lanave G, Dowdgler, Decaro N, Albanese F, Brogi E, Parisi A, Losurdo M, Lavazza A, Martella V, Buonavoglia C, Elia G. Novel orthopoxvirus and letal disease in cat, Italy.
- Osterrieder K. Familie Poxviridae. In: Selbitz H-J, Truyen U, Peter V-W, eds. Tiermedizinische Mikrobiologie, Infektions- und Seuchenlehre. 9. Auflage. Stuttgart: Enke-Verlag. 2011;420-434.
- Schaudien D, Meyer H, Grunwald D et al. Concurrent infection of a cat with cowpox virus and feline parvovirus. J Comp Pathol. 2007;137:151–4.
- Schöniger S, Chan DL, Hollinshead M et al. Cowpox virus pneumonia in a domestic cat in Great Britain. Vet Rec. 2007;160:522–3.
- Schulze C, Alex M, Schirrmeier H et al. Generalized fatal Cowpox virus infection in a cat with transmission to a human contact case. Zoonoses Public Hlth.2007; 54:31–7
- Schupp P, Pfeffer M, Meyer H, Burck G, Kolmel K, Neumann C. Cowpox virus in a 12-year-old boy: rapid identification by an orthopoxvirus-specific polymerase chain reaction. Brit J Dermatol 2001;145:146-150
- Stagegard J, Kurth A, Stern D, Dabrowski PW, Pocknell A, Nitsche A, Schrick L. Seasonal recurrence of cowpox virus outbreaks in captive cheetahs (Acinonyx jubatus). PLOS One; 2017; 12(11)e0187089.