CASE III: P16-282 (JPC 4082545)
Signalment:
4-year-old female horse (Equus caballus)
History:
Pigmented hairless mass in the skin of the pinna
Gross Pathology:
1 cm diameter white mass in the skin
Laboratory results:
No laboratory findings reported.
Microscopic Description:
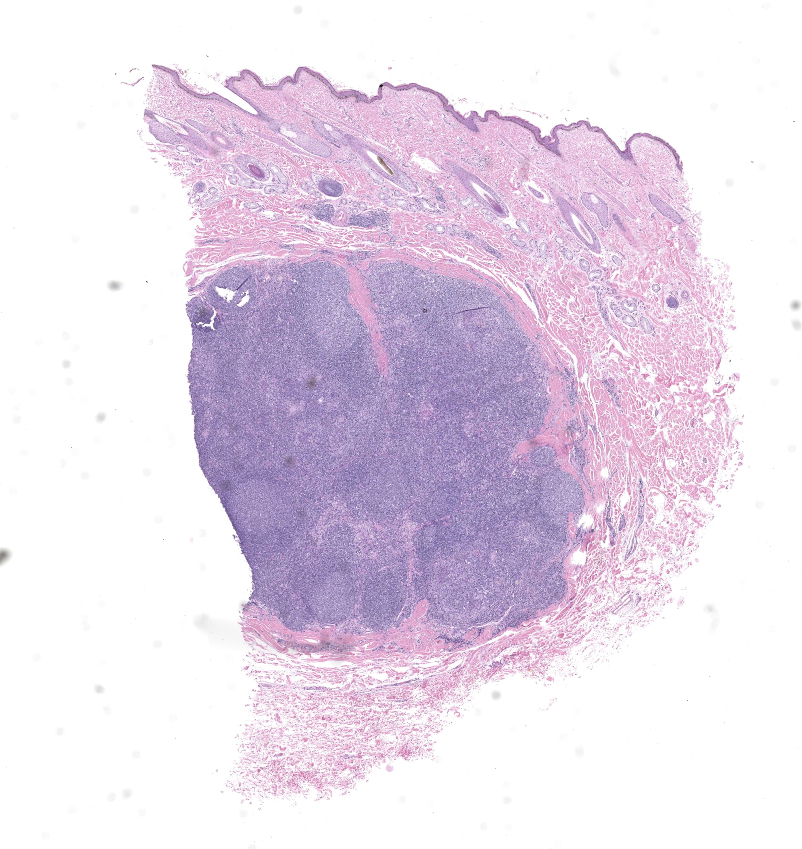
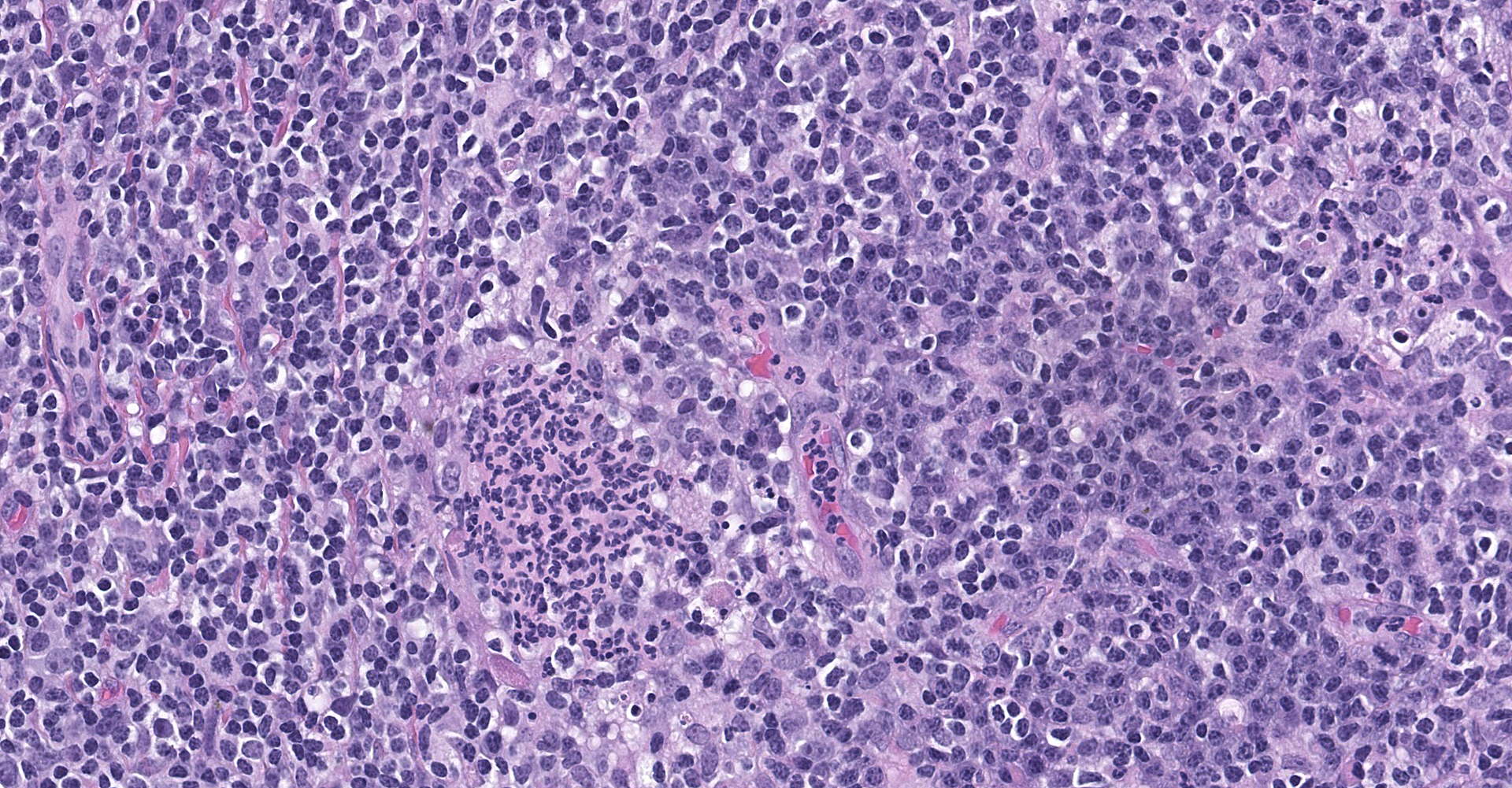
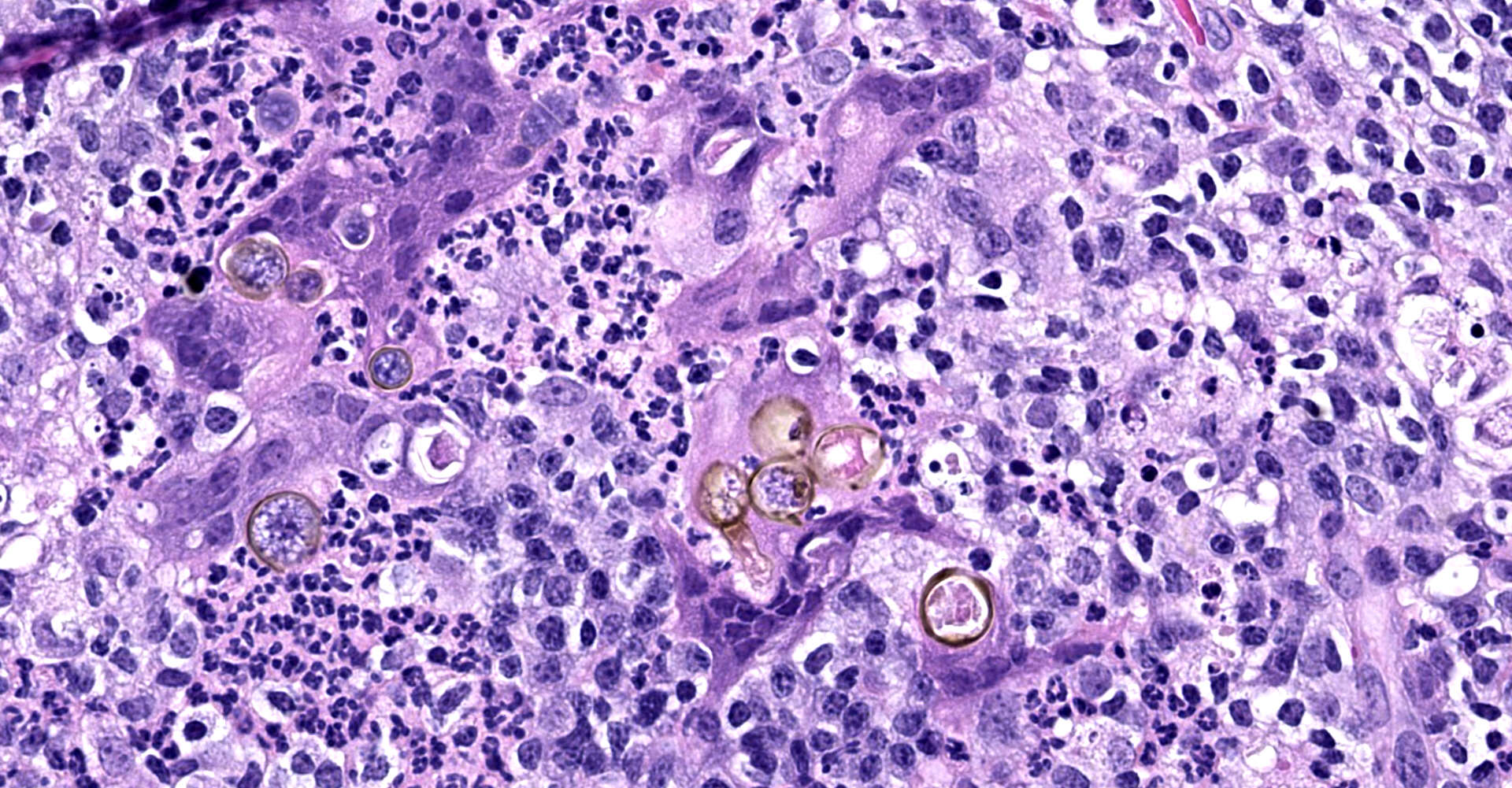
The dermis contains a well-delineated nodule composed of lymphocytes that form follicles, some with germinal centers. Dispersed throughout the lymphoid tissue are collections of macrophages, neutrophils and multinucleate giant cells. The macrophages and giant cells contain pigmented fungal organisms, forming round, yeast-like bodies, 10-30 microns in diameter, and thin septate hyphae.
Contributor?s
Morphologic Diagnoses:
Cutaneous
phaeohyphomycosis.
Contributor?s Comment:
Phaeohyphomycosis is an infection with the pigmented fungi of the family Dematiaceae.4 This family includes several genera of which Alternaria, Cladophialophora, and Curvalaria are the most common ones occurring in animals. Infections have been reported in skin, brain, nasal cavity, mucosal surfaces and systemically. These organisms are saprophytes that reside in soil, water, and decaying vegetable matter. They gain entrance into the tissue through a wound. A compromised immune system may be another factor associated with infection.
The skin is the most common site of phaeohyphomycosis in the horse and Alternaria is the most common genus isolated.2 The infection in the horse often has a pronounced lymphocytic reaction as in this case.
Contributing Institution:
College of Veterinary Medicine
Virginia Tech
Blacksburg, VA 24061
JPC
Diagnosis:
Haired skin: Dermatitis, pyogranulomatous and lymphocytic, nodular, severe, with dematiaceous yeasts and hyphae.
JPC Comment:
Dematiaceous fungi are most commonly found in the environment as plant pathogens, saprophytes, or colonizing rocks. Although these melanized fungi rarely infect vertebrates, opportunistic infections occur worldwide and have been reported in amphibians, reptiles, birds, fish, humans, and domestic animals causing a wide range of clinical conditions. These organisms are not considered as emerging opportunists in immunocompromised or otherwise debilitated vertebrates; in contrast, infections occur in healthy individuals.5
In domestic species, phaeohyphomycosis has been reported most frequently in cats and occasionally in horses, dogs, cattle, and goats. Gross lesions typically consist of single or multiple subcutaneous nodules that may be pigmented and are often mistaken for melanocytic neoplasms. Affected felines typically develop solitary lesions on the face and paws whereas horses tend to develop multiple nodules located on different parts of the body. Histologically, phaeohyphomycosis is characterized by pigmented hyphae within tissue that are associated with nodular-to-diffuse pyogranulomatous dermatitis and panniculitis.3
Factors that likely contribute to their pathogenicity include the presence of melanin and carotene, formation of thick cell walls, presence of yeast-like phases, thermotolerance, adhesion, hydrophobicity, and production of siderophores.5
Both innate and adaptive immune responses are required for effective containment of dematiaceous fungal infections. Although melanin may facilitate the organism?s evasion of the host?s defense mechanisms, it has also been reported to play a role in activating both the humoral and cellular immune responses. In addition, melanin may play a role in the activation of Toll-like receptor (TLR)-4 and induce production of the proinflammatory cytokine interleukin (IL)-8. Host defense predominantly relies upon ingestion and elimination of fungal cells by the cells of the innate immune system, especially neutrophils and macrophages. Many cases are associated with a characteristic pyogranulomatous reaction, usually indicating incomplete or frustrated phagocytosis, which means phagocytic cells are unable to efficiently phagocytize fungal cells, leading to in-situ persistence.5
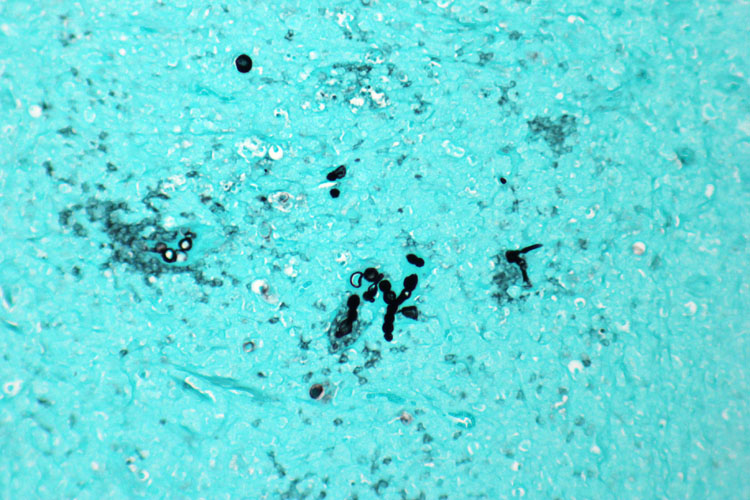
Pigmented fungi may be readily apparent during histological examination,
however, histochemical stains such as Grocott-Gomori?s methenamine silver (GMS)
and Fontana-Masson?s enhance the detection of fungal walls and melanin,
respectively. Regardless, identification of most dematiaceous fungi cannot be
achieved based on histomorphologic features alone. Culture is often required
for definitive identification3; however, culture isolates are
frequently misidentified.5 This emphasizes the important role of
molecular identification of these rare mycoses and the benefits of sequencing
as the gold standard for accurate identification.5
As noted by the contributor, the organisms responsible for phaeohyphomycosis are numerous and include (but are not limited to) the following genera: Alternaria, Bipolaris, Cladosporium, Curvularia, Exophiala, Phialophora, and Wangiella.3
Conference participants briefly discussed the value of using special stains, such as GMS, to aid in the differentiation of phaeohypho-mycosis from chromoblastomycosis. Both conditions are caused by dematiaceous fungal etiologies. Chromoblastomycosis is characterized by 4-15µm diameter, round, pigmented yeast that are also known as sclerotic bodies, chromo bodies, and Medlar bodies. In contrast, phaeohyphomycosis is characterized by pigmented fungi with both mycelial and yeast morphologies in tissue sections.3
References:
1. Arcobello JT, Revankar SG. Phaeohyphomycosis. Semin Respir Crit Care Med. 2020;41(1):131-140.
2. Genovese LM, Whitbread TJ, Campbell CK. Cutaneous nodular phaeohyphomycosis in five horses associated with Alternaria alternatal infection. Vet Rec. 2001;148(2):55-56.
3. Mauldin EA, Peters-Kennedy J. Integumentary system. In: Maxie MG ed. Jubb, Kennedy, and Palmer?s Pathology of Domestic Animals. Vol 1. 6th ed. Philadelphia, PA: Elsevier Ltd. 2016:646-7, 653, 654-5.
4. Seyedmousavi S, Guillot J, de Hoog GS. Phaeohyphomycosis, emerging opportunisitic diseases in animals. Clin Microbiol Rev. 2013;26(1):19-35.
5. Velázquez-Jiménez Y, Hernández-Castro R, Romero-Romero L, Salas-Garrido CG, Martínez-Chavarría LC. Feline Phaeohyphomycotic Cerebellitis Caused by Cladosporium cladosporioides-complex: Case Report and Review of Literature. J Comp Pathol. 2019;170:78-85.