Signalment:
Gross Description:
The gastric mucosa contained multifocal chronic ulcerations of the non-glandular mucosa, the fundus, and the margo plicatus and were characterized by elevated fibrous marginsand a dry appearance. Moderate hyperplasia of the mucosa was noticed in the proximal duodenum and right dorsal colon.
Moderate, diffuse, lymphadenomegaly, with a wet and whitish cut surface indicating a reactive lymphadenitis, was noticed in the gastric, pancreatic and mesenteric lymph nodes.
Macroscopic diagnoses: - Dermatitis, hyperplastic, exfoliative, and parakeratotic, diffuse, chronic, severe, with multifocal alopecia.
- Pancreatitis, sclerosing, diffuse, chronic, severe.
- Cheilitis, stomatitis and gastritis, ulcerative, multifocal, chronic, severe.
Histopathologic Description:
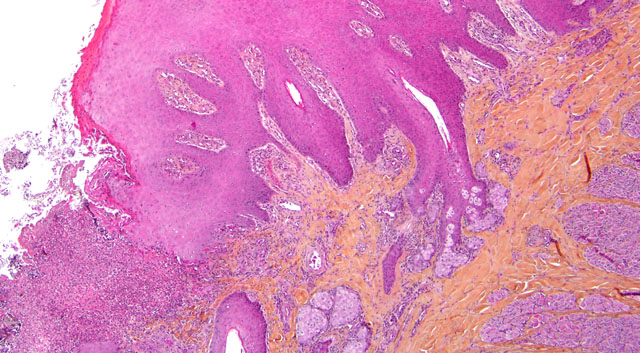
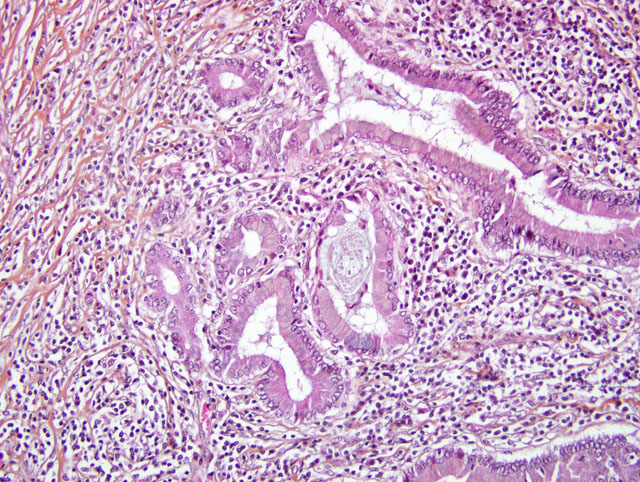
Pancreas: The architecture of the pancreatic parenchyma is completely distorted and characterized by severe, diffuse, fibrosis containing thick mature collagen fibers and few fibroblasts. Only a few pancreatic epithelial cells and islets ofLangerhansareobservedinthesections. Severeductular hyperplasia with columnar to cubioidal monostratified epithelium and abundant intraluminal amphophilic amorphous material (mucus) can be noticed. Severe multifocal infiltration by numerous non-degranulated and degranulated eosinophils, as well as lymphocytes and plasma cells, is one of the main features of this lesion. Vascular fibrosis and lymphocytic eosinophilic transcytosis are further observed features.
Colon (histoslides not submitted): The colonic crypts are separated by severe infiltration by lymphocytes, plasma cells and a few eosinophils, and are multifocally atrophic and degenerate with superficial enterocyte loss. Further, the middle sized arterioles exhibit vacuolar degeneration of the medial cells with formation of multifocal intimal and intramedial calcification foci (intimal bodies).
Morphologic Diagnosis:
1. Skin: Dermatitis, interface and perivascular, lymphoplasmacytic and eosinophilic, diffuse, chronic, severe, with focal ulceration and suppuration.
2. Pancreas: Pancreatitis, eosinophilic and sclerosing, diffuse, chronic, severe with subtotal epithelial atrophy, ductular hyperplasia and moderate multifocal lymphocytic infiltration.
3. Colon: Colitis, lymphoplasmacytic and eosinophilic, diffuse, severe, chronic with superficial epithelial erosion.
Lab Results:
Complete Blood Count:
| Parameter |
Value |
Normal Value |
| Hematocrit (%) | 5 | 32-52 |
| Hemoglobin (g/100ml) | 17.3 | 11-19 |
| Leucocytes (cells/mm3 | 12,040 | 6,000-12,500 |
| Neurophils (cells/mm3 | 8,416 | 2,000-5,500 |
| Eosinophils (cells/mm3 | 626 | 0-700 |
| Basophils (cells/mm3 | 24 | 6,000-100 |
| Monocytes (cells/mm3 | 253 | 0-600 |
| Lymphocytes(cells/mm3 | 2,661 | 1,600-4,600 |
| Thrombocytes (cells/mm3 | 175,000 | 90,000-350,000 |
Biochemical Analysis:
| Parameter |
Value |
Normal Value |
Total bilirubin | 7.8 | 0-35 |
|
| Calcium (mg/l) | 117.6 | 107-129 |
| Creatinine (mg/l) | 11.2 | 8-22 |
| GGT (Gamma glutamyl transferase) (UI/l) | 23 | 0-40 |
| Total protein (g/l) | 66 | 56-79 |
| Urea (g/l) | 0.43 | 0.1-0.24 |
| AST (UI/l) | 193 | 100-600 |
| Fibrinogen (g/l) | 3.25 | 2-4.5 |
Condition:
Contributor Comment:
Idiopathic hypereosinophilic syndrome has been reported in humans, dogs, cats, horses, and ferrets.(2,7,13) The hypereosinophilic syndrome in man is characterized by marked peripheral eosinophilic infiltrates in various organs of which the skin is the second most common. The most frequently affected organ is the heart.(8) Immunosuppressive doses of systemic glucocorticoids (dexamethasone) may be effective in horses if administered early in the course of the disease (before wasting).(3,7,11) Hydroxyurea is an orally active antineoplastic agent whose mode of action is to inhibit DNA synthesis without affecting RNA or protein synthesis; it has been used successfully for treating humans with hypereosinophilic syndrome and has been suggested for the treatment of cats. An improvement of the clinicopathological signs was noticed in a horse treated with corticosteroid and hydroxyurea and suggests that this therapy could be effective in attempts to treat this condition.(7)
JPC Diagnosis:
1. Pancreas: Pancreatitis, sclerosing, lymphoplasmacytic and eosinophilic, diffuse, marked with ductular hyperplasia, duct ectasia, and mucinous metaplasia.
2. Haireds kinand mucocutaneous junction, lip: Dermatitis and cheilitis, lymphoplasmacytic and eosinophilic, perivascular, multifocal, mild to moderate, with ulceration, epidermal hyperplasia and parakeratotic hyperkeratosis.
Conference Comment:
The moderator provided several useful guidelines for approaching the histologic evaluation of the tissues submitted for this case to arrive at the most accurate diagnosis. Many conference participants struggled with tissue identification for the pancreas due to the extensive fibrosis that replaces almost all of the glandular components. To address this difficulty, the moderator suggested first evaluating the section of skin to identify the histologic features of the lesion and develop a histomorphologic diagnosis. Knowledge of the key histologic features in the skin lesion then provides insight into the underlying disease process and pathogenesis, and then leads the astute diagnostic pathologist to consider the other tissues likely to be affected in equine multisystemic eosinophilic disease, such as the pancreas. The moderator noted that lymphoplasmacytic and eosinophilic pancreatitis and exfoliative dermatitis are classic lesions of MEED.
The contributor indicates the pathogenesis of MEED is unknown, and lists some potential etiologies. In addition to the etiologies listed, it has also been suggested that clonal proliferation of epitheliotropic T-lymphocytes in affected tissues results in secretion of interleukin-5, thereby attracting eosinophils. Another potential etiology is repeated type I hypersensitivity reactions that occur in response to inhaled, ingested (dietary), or parasitic antigens.5 The contributor provides excellent information on MEED. For additional information on other causes of eosinophilic dermatitis in horses the reader is referred to WSC 2009-2010, Conference 4, Case I.
References:
2. Carmalt J. Multisystemic eosinophilic disease in a Quarter horse. Equine Veterinary Education. 2004;16:231-234.
3.Fadok VA. An overview of equine dermatoses characterized by scaling and crusting. Vet Clin North Am Equine Pract. 1995;11:43-51. 4. Gibson KT, Alders RG. Eosinophilic enterocolitis and dermatitis in two horses. Equine Vet J. 1987;19:247-252.
5. Ginn PE, Mansell JEKL, Rakich PM. Skin and appendages. In: Maxie MG, ed. Jubb, Kennedy and Palmers Pathology of Domestic Animals. 5th ed., vol. 1. Philadelphia, PA: Elsevier Ltd; 2007:739-741.
6. Henson FMD, Milner P+â-Å, Sheldon O. Multisystemic eosinophilic epitheliotropic disease in a welsh pony. Equine Veterinary Education. 2002;14:176-178.
7. Hillyer MH, Mair TS. Multisystemic eosinophilic epitheliotropic disease in a horse: attempted treatment with hydroxyurea and dexamethasone. Vet Rec. 1992;130:392-395.
8. McCue ME, Davis EG, Rush BR, Cox JH, Wilkerson MJ. Dexamethasone for treatment of multisystemic eosinophilic epitheliotropic disease in a horse. J Am Vet Med Assoc. 2003;223:1320-1323.
9. Nimmo Wilkie JS, Yager JA, Nation PN, Clarck EG, Townsend HG, Baird JD. Chronic eosinophilic dermatitis: a manifestation of a multisystemic, eosinophilic, epitheliotropic disease in five horses. Vet Pathol. 1985;22: 297-305.
10. Sanford SE. Multisystemic eosinophilic epitheliotropic disease in a horse. Can Vet J. 1989;30: 253-254.
11. Scott DW. Unusual immune-mediated skin diseases in the horse. Equine practice. 1991;13:10-18.
12. Scott DW, Miller WH. Miscellaneous skin diseases: multisystemic eosinophilic epitheliotropic disease. In: Equine dermatology. Philadelphia, PA: WB Saunders Company; 2003:661-695.
13. Singh K, Holbrook TC, Gilliam LL, Cruz RJ, Duffy J, Confer AW. Severe pulmonary disease due to multisystemic eosinophilic epitheliotropic disease in a horse. Vet Pathol. 2006;43:189-193.