Results
AFIP Wednesday Slide Conference - No. 1
8 September 1999
- Conference Moderator:
- COL William Inskeep II
Diplomate, ACVP
Chairman, Department of Veterinary Pathology
Deputy Director, Armed Forces Institute of Pathology
Washington, DC 20306
-
- NOTE: Click on images for larger views. Use
browser's "Back" button to return to this page.
Return to WSC Case Menu
-
-
- Case I - 96-4834 (AFIP 2597320)
-
- Signalment: Neonatal bovine.
-
- History: Seven of 70 calves had diarrhea.
Laboratory Results: Florescent antibody testing was positive
for coronavirus and negative for rotavirus. Coronaviruses were
found by electron microscopy on negatively stained preparations
of colonic content.
No significant bacteria were isolated. Indirect florescent antibody
examination for E. coli K99 pilus antigen was negative. Examination
of colonic content smears was negative for Cryptosporidium sp.
by volusol AF stain.
-
- Contributor's Diagnoses and Comments:
- 1. Enteritis, ulcerative, viral, coronavirus.
- 2. Colitis, ulcerative, viral, coronavirus.
- The small intestine has marked shortening of the villi and
flattened villous epithelium. Crypt epithelium has prominent
regeneration. The colon has concurrent degeneration and regeneration
of crypt epithelium.
-
- AFIP Diagnoses:
- 1. Small intestine: Enteritis, erosive and necrotizing, acute,
diffuse, moderate, with blunting and fusion of villi, crypt abscesses,
and regeneration. breed unspecified bovine calf.
- 2. Large intestine: Colitis, erosive and necrotizing, acute,
diffuse, moderate, with crypt abscesses and regeneration.
-
- Conference Note: The main infectious causes of neonatal
calf diarrhea are rotavirus, coronavirus, enterotoxigenic Escherichia
coli, Salmonella species, and Cryptosporidium sp. Clinical differentiation
is difficult because the potential pathogens cause similar clinical
signs and frequently two or more causative agents are present.
-
- Coronavirus causes both upper respiratory and intestinal
infections, with intestinal infections occurring generally between
one and two weeks of age. Viral replication begins in the epithelium
of the proximal small intestine and spreads throughout the small
and large intestines causing necrosis of crypts and villi.
· Clinical signs: Profuse watery diarrhea, dehydration.
· Gross lesions: Mild fibrinous enterocolitis and edema
in lymph nodes.
· Pathophysiology: Infection via fecal/oral or nasal/oral
route Þ replication in oral mucosa Þ swallowed Þ
tips of villi.
· Clinical pathology: Acidosis, hyperkalemia, and hyponatremia.
· Comparative pathology: The same coronavirus is responsible
for winter dysentery in older cattle; other coronaviruses cause
feline infectious peritonitis, vomiting and wasting disease of
swine, transmissible gastroenteritis of swine and hepatitis in
mice.
Rotavirus produces enteric infection as early as three days of
age and as late as about 3 weeks of age. The lower small intestine
is generally affected. Lesions are histologically similar to
those seen in coronaviral enteritis. E. coli enterotoxicosis
occurs in calves up to 6 days of age. Diarrhea results from the
release of thermostabile enteroxin that produces profound hypersecretion
from enterocytes without significantly damaging the epithelium.
Salmonella sp. generally infect calves between one and seven
weeks of age. These bacteria damage the mucosa through invasion
and the production of enterotoxins. Infection frequently results
in septicemia. Cryptosporidium sp. Infect calves in the first
three weeks of life. These extracellular protozoa attach to the
epithelium of the small and large intestine and displace the
microvilli.
-
- Contributor: California Veterinary Diagnostic Laboratory
System, U.C. Davis, 105 West Central Avenue, San Bernardino,
CA 92408
References:
- 1. Jones T C, Hunt R D, King N W: Diseases caused by viruses.
In: Veterinary Pathology, 6th Ed, 1997, pp. 281-286.
2. Vermunt JJ: Rearing and management of diarrhoea in calves
to weaning. Australian Vet Journ. Vol. 71, No. 2, 33-41, February
1994.
3. Barker, IK, Van Dreumel, AA: The alimentary system. In: Pathology
of Domestic Animals, Vol 2. Jubb, KVF, Kennedy, PC, and Palmer,
N 4th Ed, 1993, pp 184-192.
5. Janke BH: Protecting calves from viral diarrhea. Vet Med 803-811,
August 1989.
-
-
- Case II - Case 2/BE2D/NIEHS (AFIP 2677917)
-
- Signalment: 8-week-old, female, Fischer 344 rat
-
- History: The rat was treated once daily for 2 days
by gavage with an ethylene glycol ether (EGE).
-
- Gross Pathology: No significant gross abnormalities
noted.
-
- Laboratory Results: None.
Contributor's Diagnoses and Comments:
- 1. Nasal cavity, maxillo- and nasoturbinates, submucosal
vessels - thrombosis.
- 2. Nasal cavity, incisor teeth, dental pulp - thrombosis.
In rats exposed for 2 days, disseminated thrombosis was noted
in the liver, teeth, heart, and bone marrow (in the tail and
femur) and in the lungs. Infarction was noted in the bone and
bone marrow. Use of this EGE in rats was associated with a wide
range of hematologic and pathological abnormalities (Ghanayem
1996). Blood smears obtained from exposed rats had significant
alteration of erythrocyte morphology. These changes included
stomatocytosis, spherocytosis, fragmentation of erythrocytes,
formation of ghost cells, and vesciculation. It is suggested
that chemical exposure induced either primary anemia, leading
to anoxic endothelial injury or alternatively induced changes
in the erythrocyte morphology, resulting in spherocytosis and
contributing to compromised blood flow. Either of these events
may have triggered acute disseminated intravascular coagulation
(DIC) and eventual bone infarction.
-
- AFIP Diagnosis: Nasal mucosa and dental pulp: Fibrin
thrombi, Fischer 344 rat, rodent.
-
- Conference Note: Various mechanisms that may be involved
in the pathogenesis of chemically induced thrombosis were discussed,
including vascular damage, induction of a hypercoagulable state,
and disturbance of blood flow.
Disseminated thrombosis (disseminated intravascular coagulation
(DIC) or consumption coagulopathy) is a thrombohemorrhagic disorder
that may develop as a complication in a variety of diseases.
Two mechanisms for triggering DIC are 1. Release of procoagulant
tissue factor(s) into the circulation following injury and 2.
Activation of factor XII following widespread endothelial injury
and resulting surface contact with collagen. The thrombi may
be formed in the general circulation or may be localized to a
specific organ or tissue. The thrombi may cause ischemia of more
severely affected or more vulnerable organs.
Nyska et al. reported that 2-butoxyethanol (BE) (ethylene glycol
monobutyl ether) can produce disseminated thrombosis and bone
infarction in female rats. The authors did not know the pathogenesis
of BE-induced disseminated thrombosis, but proposed that BE-induced
hemolysis (and release of procoagulant factors from damaged erythrocytes)
may result in thrombosis via disturbances of blood flow, but
direct endothelial damage and other mechanisms were also possible.
The primary support for hemolysis being the underlying cause
of DIC stems from studies that have shown that female rats are
more susceptible to BE-induced hemolysis; thrombosis and bone
infarction are observed only in female rats.
-
- Contributor: National Institute of Environmental Health
Sciences, P.O. Box 12233, Research Triangle Park, NC 27709
-
- References:
- 1. Ghanayem B: An overview of the hematoxicity of ethylene
glycol ethers. Occupat Hyg 2:253-268, 1996
2. Nyska A, et al: Disseminated thrombosis and bone infarction
in female rats following inhalation exposure to 2-butoxyethanol.
Tox Path 27(3):287-294, 1999
-
-
- Case III - 98N061 GUH DC 20007 (AFIP 2681360)
- Signalment: Two-year-old male, neutered, skunk, Mephitis
mephitis
-
- History: This skunk presented with a 2 cm diameter
ulcerated lesion on its back, duration unknown. The entire lesion
was excised and submitted for histopathology. The skunk is alive
and doing well.
-
- Gross Pathology: This two cm diameter lesion was dark
brown-black and ulcerated. It extended 1cm down into the dermis.
-
- Laboratory Results: None.
-
- Contributor's Diagnosis and Comments: Low grade leiomyosarcoma
- The H and E stained section of the mass shows that it is
composed of homogeneous round to spindloid cells arranged in
cords and short bundles embedded in a myxomatous to focally hemorrhagic
matrix. The cells are characterized by oval nuclei, 1-2 indistinct
nucleoli and scant eosinophilic cytoplasm. The mitotic rate is
low: 0-1per high power field. The overlying skin is ulcerated
with mild to moderate mixed inflammation. With the H and E stained
section alone, this neoplasm was diagnosed as a low grade sarcoma,
with leiomyosarcoma and neurofibrosarcoma included in the differential
diagnosis.
-
- Immunohistochemistry (avidin-biotin immunoperoxidase method)
was performed utilizing monoclonal antibodies to desmin, muscle
specific actin (MSA), myoglobin, S-100 protein and neuron specific
enolase (NSE). The tissue was positive for desmin and MSA, and
nonspecific for myoglobin and NSE. There were occasional positive
cells for S-100 but these were of uncertain significance. Therefore,
this mass was determined to be a leiomyosarcoma. Leiomyosarcomas
of the subcutaneous tissue are rare tumors of domestic animals.
They are speculated to originate from the smooth muscle of vessel
walls or arrrector pili muscle.
-
- AFIP Diagnosis: Haired skin and subcutis: Leiomyosarcoma,
skunk (Mephitis mephitis), mustelid.
-
- Conference Note: Cutaneous leiomyosarcomas are rarely
reported in animals. These tumors may be underdiagnosed because
of their resemblance to more common spindle cell sarcomas. The
distinguishing histologic features in this case include cells
forming long streams and bundles, end to end rowing of nuclei,
blunt-ended and occasionally plicated nuclei, moderate amounts
of variably vacuolated cytoplasm, and minimal collagenous stroma.
-
- Immunohistochemistry performed at the AFIP confirmed that
the neoplastic cells are positive for smooth muscle actin, and
negative for glial fibrillary acidic protein. Unfortunately,
immunostains for S-100 protein did not work properly on two attempts.
The AFIP's Department of Soft Tissue Pathology reviewed this
case and favored a diagnosis of epithelioid leiomyosarcoma. In
humans and animals, cutaneous leiomyosarcomas are generally low-grade
malignancies.
Contributor: Georgetown University/DCM, 3950 Reservoir
Rd. NW, Washington, DC 20007
-
- References:
- 1. Brunnert SR, Herron AJ, and Altman NH: Leiomyosarcoma
in a domestic ferret: morphologic and immuncytochemical diagnosis.
Lab Ani Sci, vol 40, no. 2:208-209, 1990.
- 2. Brunnert SR, Herron AJ, and Altman NH: Leiomyosarcoma
in a Peruvian squirrel monkey (Saimiri sciureus). Vet Pathol,
vol. 27:126-128, 1990.
- 3. Gross TL, Ihrke PJ, Walder EJ: Veterinary Dermatopathology,
pp. 444-445. Mosby-Year Book Inc, St Louis, Missouri, 1992.
4. Hanzaike Tl, Ito I, Ishikawa T et al: Leiomyosarcoma of soft
tissue in a cow. J Comp Path, vol.112:237-242, 1995.
- 5. Sartin EA, Doran SE, Riddell MG et al: Characterization
of naturally occurring cutaneous neurofibromatosis in Holstein
cattle. Am J Pathol, vol 145, no. 15:1168-1174, 1994.
-
-
- Case IV - 99-0002 (H99-0065 D) (AFIP 2681727)
-
- Signalment: Fledgling Nankeen kestrel (Falco cenchroides)
-
- History: A wild Nankeen kestrel fledgling with a history
and clinical signs of episodic nervous disease, blindness, head-pressing,
intermittent seizures, loss of balance and spontaneous screaming
was presented for necropsy examination. Ophthalmological examination
demonstrated a swollen and hyperaemic pecten and mild hyphaema.
-
- Gross Pathology: There was congestion of cerebral
vessels and multifocal petechial haemorrhages in the leptomeninges
and throughout the brain parenchyma.
-
- Laboratory Results: Haematological examination demonstrated
a normal total white blood cell count with a moderate relative
lymphocytosis and heteropaenia. Occasional rare, large, round,
bluish, granular, intracytoplasmic gametocytes and eccentrically
displaced sometimes distorted nuclei in circulating leukocytes
were observed. Plasma creatine kinase concentration was slightly
elevated but other biochemical parameters were normal. Cultures
of liver and lung failed to yield bacterial isolates.
-
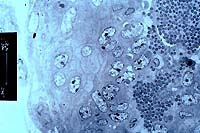
- Contributor's Diagnoses and Comments: Brain and eye:
Severe, subacute vascular endothelial hyperplasia, granulomatous
perivasculitis and pectinitis with endothelial parasitic cysts
measuring 40 to 60 mm in diameter.
-
- The lesions presented in this case are characteristic of
a disease which is seasonally common in young Western Australian
falcons (Jaensch and Raidal 1996; Raidal et al 1999). The inflammatory
lesions centered on the vessels of the brain and pecten represent
the schizogenous phase of a Leucocytozoon sp. Transmission electron
microscopy demonstrated marked proliferation of endothelial cells
and swollen endothelial cells containing abundant mitochondria.
Occasional endothelial cells contained intracytoplasmic parasitophorous
vacuoles containing granular material or larger similar vacuoles
(10-20 mm in diameter) containing electron-dense granular material,
nuclear membranes and electron-dense aggregates. Spherical protozoal
merozoites measuring 1 mm in diameter were present within thin-walled
endothelial cysts and also free within the lumens of vessels.
The zoites contained a spherical, indented nucleus measuring
0.5 mm in diameter and paired, tear-shaped, electron-dense rhoptries
and microneme-like electron-densities.
Severely affected kestrels typically have low numbers of circulating
leucocytozoon gametocytes in blood smears. Although acute disease
can occur rapidly before the completion of gametogony, endothelial
schizonts occur consistently in the arterioles of the brain,
spinal cord, optic nerve, pecten and kidney and less frequently
in arterioles of the lungs, heart, liver, intestines and spleen.
Leucocytozoon are parasites of birds and, in most species, schizogony
with the production of small schizonts, and in some species megaloschizonts,
occurs in hepatocytes or hepatic sinusoidal endothelial cells
although schizogony and gametogony can also occur in other tissues
(Steele and Noblet 1992). All affected falcons and kestrels examined
so far have had no evidence of hepatic phases of schizogony.
The predilection for arterioles in the central nervous system,
eye and kidney is unusual for Leucocytozoon species.
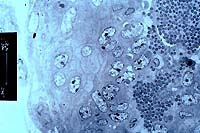
- Case 1-4. Transmission electron micrograph.
-
- AFIP Diagnoses:
- 1. Cerebrum and brain stem: Endothelial hyperplasia and hypertrophy,
multifocal, marked, with intraendothelial protozoal schizonts,
hemorrhage, and perivascular hemosiderophages, Nankeen kestrel
(Falco cenchroides), avian.
- 2. Eye: Endothelial hyperplasia and hypertrophy, multifocal,
moderate, with intraendothelial protozoal schizonts, and histiocytic
pectinitis.
Conference Note: The differential diagnosis in this case
includes Leucocytozoon sp, Hemoproteus sp., Toxoplasma gondii,
Sarcocystis sp., Plasmodium sp. and microsporidia. The size and
location of schizonts within the cytoplasm of endothelial cells
leads to a shortened differential diagnosis of Leucocytozoon
sp. and Hemoproteus sp. The presence of intraleukocytic stages
in circulating erythrocytes and leukocytes supports the final
diagnosis of Leucocytozoon sp.
-
- Contributor: Division of Biochemical Sciences, Murdoch
University, South Street Murdoch, Western Australia, 6150
-
- References:
1. Gardiner CH, Fayer R, Dubey JP: An Atlas of Protozoan Parasites
in Animal Tissues, 2nd ed., pp. 73-74. Armed Forces Institute
of Pathology, Washington, DC, 1998
- 2. Jaensch SM, Raidal SR: Neurological disease and blindness
- two case studies. Annual Proceedings of the Australian Chapter
of the Association of Avian Veterinarians., O'Reilly's Rainforest
Resort, Lamington National Park, Queensland, pp 151-154, 1996
- 3. Raidal SR, Jaensch SM, Ende J: Preliminary report of a
parasitic infection of the brain and eyes of a Peregrine Falcon
Falco peregrinus and Nankeen Kestrels Falco cenchroides in Western
Australia, EMU, 99:1-2, 1999
- 4. Steele EJ, Noblet GP: Schizogonic development of Leucocytozoon
smithi. Journ of Parasit, 39:530-536, 1992.
-
- J Scot Estep, DVM
Captain, VC, USA
Registry of Veterinary Pathology*
Department of Veterinary Pathology
Armed Forces Institute of Pathology
(202)782-2615; DSN: 662-2615
Internet: estep@afip.osd.mil
-
- * The American Veterinary Medical Association and the American
College of Veterinary Pathologists are co-sponsors of the Registry
of Veterinary Pathology. The C.L. Davis Foundation also provides
substantial support for the Registry.
-
- Return to WSC Case Menu